An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Klebsiella Pneumoniae Liver Abscess: a Case Report and Review of Literature
Faisal kamal, george williams, muhammad ali khan, dipen kadaria.
- Author information
- Article notes
- Copyright and License information
Faisal Kamal [email protected]
Corresponding author.
Received 2016 Jun 15; Accepted 2017 Jan 10; Collection date 2017 Jan.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Klebsiella pneumoniae (K.pneumoniae) is a known cause of pyogenic liver abscess (PLA) in the absence of hepatobiliary disease. In settings of hepatic infection, it has also been known to cause disseminated infections including meningitis and endopthalmitis. Several groups of patients are particularly susceptible to infection, including patients with diabetes mellitus, those from Southeast Asia and those with the preexisting hepatobiliary disease. We present a case of K.pneumoniae PLA with bacteremia. A 39-year-old Vietnamese male with no previous medical history who presented with complaints of abdominal pain, nausea, vomiting, diarrhea and fever. A computed tomography (CT) of the abdomen showed a large complex mass in the right lobe of the liver with multiple septations. Over course of hospitalization, the patient developed acute respiratory failure and was monitored in medical intensive care unit (MICU). Blood cultures grew K. pneumonia. The patient was treated with intravenous ceftriaxone and the abscess was drained by interventional radiology. After appropriate management, he progressed well during his hospital course and was eventually discharged from the hospital. K. pneumonia PLA had previously been an endemic disease in Southeast Asia, however, with a highly mobile patient population, it is now seen throughout the world and should be in the differential of patients who present with solitary liver mass in the setting of sepsis.
Keywords: hepatic abscesses
Introduction
Klebsiella pneumoniae is a gram-negative organism that can cause pyogenic liver abscess (PLA) in the absence of hepatobiliary disease. Diabetics are at increased risk of this infection. Some patients with Klebsiella liver abscess can develop metastatic infections including endophthalmitis, meningitis, brain abscess, septic pulmonary emboli, lung abscess, splenic abscess, osteomyelitis, etc. It has been found to be a common cause of liver abscess in Taiwan. However, recently there has been the change in the trend of this infection in the United States [ 1 ]. And now it is one of the common causes of PLA in the United States. We present a case of Klebsiella liver abscess with bacteremia. Informed consent was obtained from the patient for this study.
Case presentation
A 39-year-old Vietnamese male with no significant past medical history presented to a large urban emergency department with complaints of sharp 5/10 right upper quadrant abdominal pain, nausea, vomiting, fever and chills. The patient stated that he had been in his previous state of good health until approximately three days prior to presentation when his symptoms became debilitating. He worked at a local nail salon and stated that several co-workers were exhibiting cold like symptoms. His travel history was significant for the trip back to Vietnam within the last year but stated that his travels were uneventful and he did not remember feeling ill during that time. Review of systems was significant for the aforementioned symptoms in addition to loss of appetite with early satiety and one previous episode of streaky hemoptysis several days prior to presentation. In the emergency department, basic laboratory showed that he had an increased anion gap to 18, an acute kidney injury with a serum creatinine of 1.4, alkaline phosphatase 172, AST 81, ALT 107, ferritin 4,680 and a white blood cell count of 10.5.
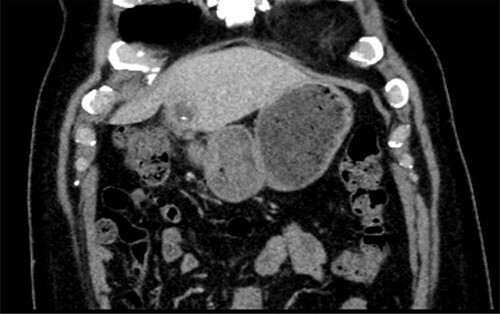
A computed tomography (CT) scan with contrast of the chest and abdomen was ordered which was significant for a large 4.3 x 4.1 x 4.5 cm complex mass in the right lobe of the liver with multiple septations. Ultrasound of the abdomen showed a heterogeneous, hypoechoic, multiseptated hepatic mass with internal vascularity, however, a neoplastic, infectious or protozoa process could not be differentiated. He was admitted to the general medicine floor, was started on vancomycin and piperacillin/tazobactam with fluid resuscitation consisting of crystalloids, and blood cultures were ordered. Shortly after admission he became tachypneic, tachycardic and hypoxic with oxygen saturations in the 50s. At that time, he was placed on high-flow oxygen and had a rebound of his oxygen saturations to the low 90s, but still remained tachypneic and tachycardic. At this time, it was determined that he would benefit from admission to the medical intensive care unit (MICU). An arterial blood gas (ABG) was obtained and was significant for a pH of 7.34, a pCO2 of 26, and a bicarbonate of 14. He was placed on bilevel positive airway pressure ventilation and was continued on his antibiotics.
The repeat CT of thorax and abdomen was again significant for a large, complex hepatic mass, but now showed areas of consolidated infiltrate with some associated atelectatic change in the posterior right lower lobe. Magnetic resonance imaging (MRI) was recommended and showed a peripherally enhancing mass in the anterior segment of the right hepatic lobe that measured 3.5 cm x 3.3 cm with areas of central septations. Blood cultures grew Klebsiella pneumonia on the second day of admission with a MIC< 1 for ceftriaxone. He was placed on ceftriaxone and the abscess was drained by interventional radiology. The gram stain and cultures of pus were negative. The patient progressed well through his hospital course and was transferred out of the MICU after three days and from the hospital after 11 days. He was seen by infectious disease two months after discharge and a repeat CT of the abdomen showed interval improvement of the abscess.
Once thought to be isolated to Southeast Asia, pyogenic liver abscess (PLA) caused by Klebsiella pneumonia (K.pneumoniae), a potentially life-threatening cause of intra-abdominal infections in septic patients, is now seen across the World [ 2 ]. K.pneumoniae is now recognized as the most common isolate in both Asia and the USA and is seen in greater than 60% of monomicrobial and polymicrobial PLA infections [ 3 - 4 ]. The gram-negative K.pneumoniae is a well-known pathogen that is identified in multiple disease processes; however, what makes K.pneumoniae PLA unique is the patient population afflicted, its virulence and diagnostic features.
The most common presenting symptoms of K.pneumoniae PLA are fever, nausea, vomiting, and abdominal pain over the right upper quadrant. An elevated white blood cell count is almost universally seen. Asian ethnicity, recent antibiotic use, diabetes mellitus and impaired fasting blood glucose are the most important predisposing risk factors for developing K.pneumoniae PLA. Although males and those from Southeast Asia are over represented, PLA has been seen in all sexes and ethnicities. Diabetics tend to have monomicrobial abscess and disease process is typically more invasive with metastases to other organs, is often present and can lead to overwhelming sepsis. Septic endophthalmitis is strongly associated with the more virulent strains and diabetics [ 5 ]. Respiratory symptoms are often seen in invasive disease as the lungs are a common target for metastatic spread. The presence of meningitis, visual symptoms, dyspnea, cough, chest pain, large abscess size, all portend a worse prognosis and increased mortality [ 6 ].
Impaired neutrophil phagocytosis is what allows K.pneunoniae PLA to form in predisposed individuals. K1 K.pneumonia is the most commonly identified serotype seen in diabetics with invasive disease [ 5 ]. A novel gene, mapA, encoding for an outer membrane protein is commonly identified in invasive cases. Although, its exact virulence mechanism is not completely understood, when mapA is lost K.pneumoniae was susceptible to phagocytosis and became avirulent in mice. Because mapA is ubiquitous in virulent cases it could one day possibly be used as a laboratory marker for early identification in cases of suspected PLA. Hypermucoviscosity also plays a role in virulence in those with invasive disease, however, the exact mechanism of how hypermucoviscosity aides in virulence remain elusive.
Typical findings of K.pneumoniae PLA on abdominal computed tomography with contrast are a single, thin walled, multiseptated, solid masses with necrotic centers [ 7 - 8 ]. A predominately solid appearance is seen under ultrasound and aspiration often yields little pus with abundant necrotic material [ 9 ]. Monotherapy with an extended spectrum penicillins, such as piperacillin-tazobactam, or the third generation cephalosporin ceftriaxone in combination with metronidazole are first line therapies [ 10 ]. If unavailable, carbapenems or fluoroquinolones in conjunction with metronidazole can be used as second line therapy. Antibiotic resistance is more common in nosocomial infections; thankfully, however extended spectrum beta-lactamase strains (ESBL) are rarely seen. As with any abscess, prompt drainage with or without drain placement should be done early in the disease course.
Conclusions
PLA should be part of the differential diagnosis of liver mass in the setting of sepsis, as K.pneumoniae is the most common isolate from both monomicrobial and polymicrobial PLA. Diabetes mellitus is the single most important risk factor for contracting K.pneumoniae PLA. Imaging of K.pneumoniae PLA often shows a solid, multiloculated mass. K.pneumoniae PLA, in particular, has a propensity to metastasize to other organs and cause systemic symptoms, and prompt drainage along with antibiotics drastically decrease morbidity and mortality.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
- 1. Pyogenic liver abscess: recent trends in etiology and mortality. Rahimian J, Wilson T, Oram V, Holzman RS. Clin Infect Dis. 2004;39 (11):1654–1659. doi: 10.1086/425616. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Pyogenic liver abscess with a focus on Klebsiella pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics Klebsiella liver abscess. Lederman ER, Crum NF. Am J Gastroenterol. 2005;100 (2):322–331. doi: 10.1111/j.1572-0241.2005.40310.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. Yang CC, Yen CH, Ho MW, Wang JH. http://europepmc.org/abstract/med/15221038 . J Microbiol Immunol Infect. 2004;37 (3):176–184. [ PubMed ] [ Google Scholar ]
- 4. Pyogenic liver abscess: a retrospective analysis of 107 patients during a 3-year period. Chan KS, Chen CM, Cheng KC, Hou CC, Lin HJ, Yu WL. http://www.researchgate.net/profile/Weng_Liang_Yu/publication/7393199_Pyogenic_liver_abscess_A_retrospective_analysis_of_107_patients_during_a_3-year_period/links/0deec537c607853431000000.pdf . Jpn J Infect Dis. 2005;58 (6):366–368. [ PubMed ] [ Google Scholar ]
- 5. A global emerging disease of Klebsiella pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Fung CP, Chang FY, Lee SC, Hu BS, Kuo BI, Liu CY, et al. Gut. 2002;50 (3):420–424. doi: 10.1136/gut.50.3.420. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. Fang CT, Chuang YP, Shun CT, Chang SC, Wang JT. J Exp Med. 2004;199 (5):697–705. doi: 10.1084/jem.20030857. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. CT differentiation of pyogenic liver abscesses caused by Klebsiella pneumoniae vs non-Klebsiella pneumoniae. Lee NK, Kim S, Lee JW, Jeong YJ, Lee SH, Heo J, et al. Br J Radiol. 2011;84 (1002):518–525. doi: 10.1259/bjr/23004588. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. CT appearance of pyogenic liver abscesses caused by Klebsiella pneumoniae. Alsaif HS, Venkatesh SK, Chan DS, Archuleta S. Radiology. 2011;260 (1):129–138. doi: 10.1148/radiol.11101876. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Pyogenic liver abscesses caused by Klebsiella pneumoniae: US appearance and aspiration findings. Hui JY, Yang MK, Cho DH, Li A, Loke TK, Chan JC, et al. Radiology. 2007;242 (3):769–776. doi: 10.1148/radiol.2423051344. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Early diagnosis and therapeutic choice of Klebsiella pneumoniae liver abscess. Li J, Fu Y, Wang JY, Tu CT, Shen XZ, Li L, et al. Front Med China. 2010;4 (3):308–316. doi: 10.1007/s11684-010-0103-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (85.7 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Laparoscopic drainage of liver abscess: case report and literature review
- PMID: 23837960
- PMCID: PMC3915587
- DOI: 10.11138/gchir/2013.34.5.180
Aim: To evaluate the safety and efficacy of the minimally invasive surgical approach (laparoscopic drainage) of liver abscesses in selected cases.
Case report: Male, 58 years old, from a rural area, presented with epigastric abdominal pain, fever, weight loss, loss of appetite, a palpable mass in the epigastrium and neutrophilic leukocytosis. CT revealed a complex multiloculated liver abscess in segments 2-3. Systemic antibiotic therapy alone was ineffective; percutaneous drainage was excluded due to the characteristics of the lesion.
Result: Given the complexity of the lesion, a laparoscopic approach was chosen involving complete drainage of the abscess, debridement and irrigation; the cavity was unroofed using electrocautery and samples were obtained for bacterial culture and drug testing. Two drains were left in the cavity for seven days. No complications were observed.
Discussion: In accordance with the scientific literature, after thorough imaging we performed laparoscopic drainage of a large, complex liver abscess as a safe, effective alternative to open surgery when antibiotic therapy alone failed and percutaneous drainage was uncertain.
Conclusion: Not all liver abscesses can be treated with antibiotic therapy or percutaneous drainage. Laparoscopic drainage in association with systemic antibiotic therapy is a safe and effective minimally invasive approach that should be considered in selected patients.
Publication types
- Case Reports
- Anti-Bacterial Agents
- Drainage / methods*
- Laparoscopy*
- Liver Abscess / surgery*
- Middle Aged
- Search Menu
- Sign in through your institution
- Volume 2024, Issue 12, December 2024 (In Progress)
- Volume 2024, Issue 11, November 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation, learning points/take-home messages, conflict of interest statement.
- < Previous
Liver abscess secondary to fishbone ingestion: case report and review of the literature
- Article contents
- Figures & tables
- Supplementary Data
Niamh Grayson, Hiba Shanti, Ameet G Patel, Liver abscess secondary to fishbone ingestion: case report and review of the literature, Journal of Surgical Case Reports , Volume 2022, Issue 2, February 2022, rjac026, https://doi.org/10.1093/jscr/rjac026
- Permissions Icon Permissions
We report a rare silent migration of a fishbone into the liver and review the relevant literature. A 56-year-old man presented with a 2-day history of dull epigastric pain and raised inflammatory markers. Computerized tomography scan revealed a 4-cm abscess in the left lobe of the liver, with a linear radio-dense foreign body within the collection. At laparoscopy the hepatogastric fistula was disconnected. The fishbone was retrieved from the liver. Gastrostomy was closed with an omental patch. The patient had an uneventful recovery. Fifty-two cases of liver abscess secondary to enterohepatic fishbone migration were reported with over two-thirds presenting with a left-lobe abscess. There was marked variability in the management of liver abscess in the setting of fishbone migration-summarized in table. We believe that laparoscopic drainage of the abscess and extraction of the foreign body offer control of the source of sepsis and diminishes recurrence, whilst having a low-risk profile.
Foreign body ingestion is a common occurrence, majority of these pass without complications [ 1 ]. An estimated 1% of ingested foreign bodies result in gastrointestinal perforation, these are often sharp objects, such as accidentally ingested fishbones [ 2 ]. The sites of perforation vary, with the rectosigmoid or ileocolic being the most common [ 3 ].
We report a rare case of fishbone migration resulting in liver abscess and review of the literature. This was originally described in 1898 by Lambert [ 4 ].
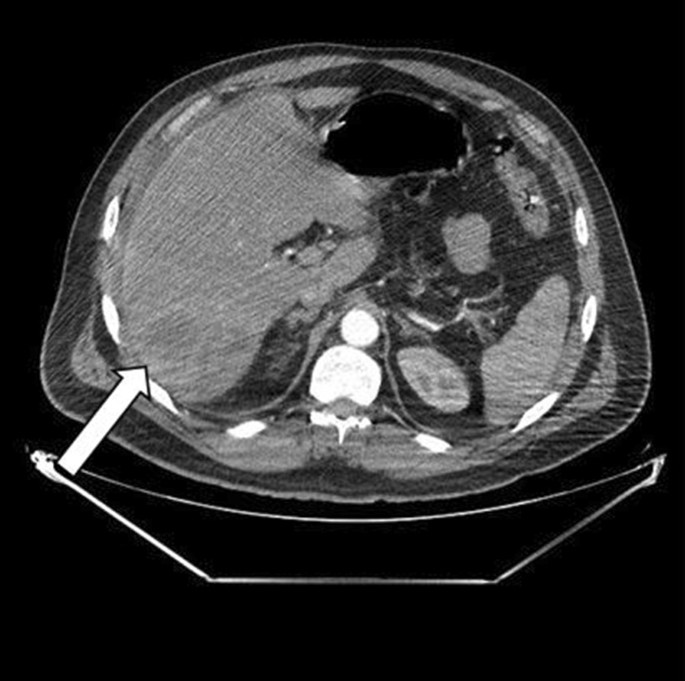
A 56-year-old man presented with a 2-day history of epigastric pain, leucocytosis and raised C Reactive Protein (CRP). A computed tomography (CT) scan revealed evidence of a 4.2 × 2.5 cm abscess in the left lobe of the liver (Segment III), with a linear radio-dense foreign body seen within the collection ( Fig. 1 ). There was fat stranding around the pylorus. The patient was treated with antibiotics in his local hospital and a trial of aspiration revealed purulent fluid. An oesphagoduodenoscopy (OGD) was normal with no evidence of foreign body or inflammation in the stomach.

CT scan showing left lobe liver abscess with fishbone.
Review of literature reported cases of enterohepatic fishbone migration
The patient was transferred to our Hepatopancreaticobiliary (HPB) unit. On arrival, he was clinically well and asymptomatic. A repeat CT scan showed a persistent collection in the liver. On further enquiry, the patient revealed that a few weeks earlier as he had a transient episode of choking and discomfort whilst eating fish.
On laparoscopy, the left lateral segment of the liver was adherent to the gastric antrum ( Fig. 2 ). Adhesions between the liver and stomach were divided with blunt and sharp dissection. The fishbone was pulled out of the liver intact and extracted through the port. The abscess was opened, drained and washed. A sealed fistulous tract was identified at the antrum; this was repaired with an omental patch. The patient had an uneventful recovery and was discharged the following day.

Fishbone extraction from the liver.
Fifty-two cases of liver abscess secondary to enterohepatic fishbone migration have been reported in the English literature ( Table 1 ). Most common symptoms included: anorexia, epigastric pain and fever. The lack of history of ingestion of a fishbone often leads to a diagnostic dilemma. CT scan was diagnostic in 47 that had axial imaging, three fishbones were found intra-operatively and two on autopsy. Over two-thirds of reported cases presented with a left lobe abscess, this is attributable to the anatomical proximity of the stomach.
There was marked variability in the management of liver abscess in the setting of fishbone migration. A variety of approaches including laparotomy, laparoscopy, CT guidance and liver resection were utilized to remove the fishbones. Percutaneous drainage usually results in the resolution of liver abscess, but recurrence is likely. Nine patients had the fishbone left in situ , one patient ultimately required a laparotomy for fishbone removal [ 5 ]. There were two mortalities in these patients with the fishbone left in situ (2/7, 29%), these were secondary to overwhelming sepsis, and the fishbones were discovered at autopsy [ 6 , 7 ].
Left lobe liver abscess should raise the suspicion of a foreign body. Antibiotic treatment and drainage are effective in the short term. The retained foreign body acts as a nidus for recurrent infection and requires removal to prevent recurrence and mortality.
Previous presentation: Poster presentation in UGI conference 2021.
None declared.
Kings College London (JISC affiliated).
Abel RM , Fischer JE , Hendren WH . Penetration of the alimentary tract by a foreign body with migration to the liver . Arch Surg. 1971 ; 102 : 227 – 8 .
Google Scholar
Horii K , Yamazaki O , Matsuyama M , Higaki I , Kawai S , Sakaue Y . Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case . Surg Today. 1999 ; 29 : 922 – 6 .
McCanse DE , Kurchin A , Hinshaw JR . Gastrointestinal foreign bodies . Am J Surg. 1981 ; 142 : 335 – 7 .
Lambert A . Abscess of the liver of unusual origin . NY Med J. 1898 ; 177 – 8 .
Masoodi I , Alsayari K , Al Mohaimeed K , Ahmad S , Almtawa A , Alomair A , et al. Fish bone migration: an unusual cause of liver abscess . BMJ Case Rep. 2012 ; 2012 :bcr0920114838.
De la Vega M , Rivero JC , Ruiz L , Suarez S . A fish bone in the liver . Lancet. 2001 ; 358 : 982 .
Theodoropoulou A , Roussomoustakaki M , Michalodimitrakis MN , Kanaki C , Kouroumalis EA . Fatal hepatic abscess caused by a fish bone . Lancet. 2002 ; 359 : 977 .
Akhondi H , Sabih DE . Liver Abscess . Treasure Island (FL) : StatPearls , 2021 .
Google Preview
Allam M , Pericleous S . Migrated fish bone induced liver abscess: medical management . Pan Afr Med J. 2020 ; 36 : 140 .
Bandeira-de-Mello RG , Bondar G , Schneider E , Wiener-Stensmann IC , Gressler JB , Kruel CRP . Pyogenic liver abscess secondary to foreign body (fish bone) treated by laparoscopy: a case report . Ann Hepatol. 2018 ; 17 : 169 – 73 .
Barkai O , Kluger Y , Ben-Ishay O . Laparoscopic retrieval of a fishbone migrating from the stomach causing a liver abscess: report of case and literature review . J Minim Access Surg. 2020 ; 16 : 418 – 20 .
Beckers G , Magema JP , Poncelet V , Nita T . Successful laparoscopic management of a hepatic abscess caused by a fish bone . Acta Chir Belg. 2021 ; 121 : 135 – 8 .
Bekki T , Fujikuni N , Tanabe K , Amano H , Noriyuki T , Nakahara M . Liver abscess caused by fish bone perforation of stomach wall treated by laparoscopic surgery: a case report . Surg Case Rep. 2019 ; 5 : 79 .
Burkholder R , Samant H . Management of fish bone-induced liver abscess with foreign body left in situ . Case Reports Hepatol. 2019 ; 2019 : 9075198 .
Chen J , Wang C , Zhuo J , Wen X , Ling Q , Liu Z , et al. Laparoscopic management of enterohepatic migrated fish bone mimicking liver neoplasm: a case report and literature review . Medicine (Baltimore). 2019 ; 98 : e14705 .
Clarencon F , Scatton O , Bruguiere E , Silvera S , Afanou G , Soubrane O , et al. Recurrent liver abscess secondary to ingested fish bone migration: report of a case . Surg Today. 2008 ; 38 : 572 – 5 .
Dangoisse C , Laterre PF . Tracking the foreign body, a rare cause of hepatic abscess . BMC Gastroenterol. 2014 ; 14 : 167 .
Dias AR , Szor DJ , Ferreira CBA , Navarro CL . Uncommon cause of liver abscess . Clin Case Rep. 2018 ; 6 : 1649 – 50 .
Ede C , Sobnach S , Kahn D , Bhyat A . Enterohepatic migration of fish bone resulting in liver abscess . Case Rep Surg. 2015 ; 2015 : 238342 .
Esseghaier S , Nassej O , Haouas N , Benhassen I , Maamar AB , Daghfous MH . Liver abscess caused by migration of an ingested foreign body . Presse Med. 2015 ; 44 : 851 – 3 .
Fujiwara Y , Shiba H , Nakabayashi Y , Otsuka M , Yanaga K . Hepatic abscess in the Spiegel lobe caused by foreign body penetration: report of a case report . Surg Case Rep. 2017 ; 3 : 24 .
Gaba RC , Bui JT , Carroll RE . Catch of the day: forceps removal of embedded fish bone . J Vasc Interv Radiol. 2013 ; 24 : 1545 .
Goh BK , Yong WS , Yeo AW . Pancreatic and hepatic abscess secondary to fish bone perforation of the duodenum . Dig Dis Sci. 2005 ; 50 : 1103 – 6 .
Gomez Portilla A , Ezurmendia B , Martin E , Lopez de Heredia E , Muriel LJ . Fish bone-related intrahepatic abscess. An underdiagnosed condition? Cir Esp (Engl Ed). 2019 ; 97 : 116 – 8 .
Goyal P , Gupta S , Sapire J . Bone causing abdominal groans . J Emerg Med. 2019 ; 57 : e95 – e7 .
Hernandez-Villafranca S , Qian-Zhang S , Garcia-Olmo D , Villarejo-Campos P . Liver abscess due to a fish bone injury: a case report and review of the literature . Cir Cir. 2020 ; 88 : 1 – 4 .
Jarry J , Nguyen V , Stoltz A , Imperato M , Michel P . A fish bone-related hepatic abscess . Clin Pract. 2011 ; 1 : e115 .
Kadowaki Y , Tamura R , Okamoto T , Mori T , Mori T . Ruptured hepatic abscess caused by fish bone penetration of the duodenal wall: report of a case . Surg Today. 2007 ; 37 : 1018 – 21 .
Kosar MN , Oruk I , Yazicioglu MB , Erol C , Cabuk B . Successful treatment of a hepatic abscess formed secondary to fish bone penetration by laparoscopic removal of the foreign body: report of a case . Ulus Travma Acil Cerrahi Derg. 2014 ; 20 : 392 – 4 .
Lau CW , Wong KM , Gogna A . Image-guided percutaneous transhepatic removal of fish bone from liver abscess . J Radiol Case Rep. 2017 ; 11 : 1 – 7 .
Lee KF , Chu W , Wong SW , Lai PB . Hepatic abscess secondary to foreign body perforation of the stomach . Asian J Surg. 2005 ; 28 : 297 – 300 .
Li J , Zhao D , Lei L , Zhang L , Yu Y , Chen Q . Liver abscess caused by ingestion of fishbone: a case report . Medicine (Baltimore). 2019 ; 98 : e16835 .
Liang H , Liu OQ , Ai XB , Zhu DQ , Liu JL , Wang A , et al. Recurrent upper quadrant pain: a fish bone secondary to gastric perforation and liver abscess . Case Rep Gastroenterol. 2011 ; 5 : 663 – 6 .
Mateus JE , Silva C , Beirao S , Pimentel J . Hepatic abscess induced by fish bone migration: two case reports . Acta Med Port. 2018 ; 31 : 276 – 9 .
Matrella F , Lhuaire M , Piardi T , Dokmak S , Bruno O , Maestraggi Q , et al. Liver hilar abscesses secondary to gastrointestinal perforation by ingested fish bones: surgical management of two cases . Hepatobiliary Surg Nutr. 2014 ; 3 : 156 – 62 .
Ng CT , Htoo A , Tan SY . Fish bone-induced hepatic abscess: medical treatment . Singapore Med J. 2011 ; 52 : e56 – 8 .
Panebianco A , Lozito RC , Prestera A , Ialongo P , Volpi A , Carbotta G , et al. Unusual liver abscess secondary to ingested foreign body: laparoscopic management . G Chir. 2015 ; 36 : 74 – 5 .
Peixoto A , Goncalves R , Macedo G . Liver abscess associated sepsis caused by fish bone ingestion . GE Port J Gastroenterol. 2016 ; 23 : 322 – 3 .
Perera MT , Wijesuriya SR , Kumarage SK , Ariyaratne MH , Deen KI . Inflammatory pseudotumour of the liver caused by a migrated fish bone . Ceylon Med J. 2007 ; 52 : 141 – 2 .
Queiroz RM , Filho FB . Liver abscess due to fish bone ingestion . Pan Afr Med J. 2019 ; 32 : 26 .
Santos SA , Alberto SC , Cruz E , Pires E , Figueira T , Coimbra E , et al. Hepatic abscess induced by foreign body: case report and literature review . World J Gastroenterol. 2007 ; 13 : 1466 – 70 .
Sim GG , Sheth SK . Retained foreign body causing a liver abscess . Case Rep Emerg Med. 2019 ; 2019 : 4259646 .
Tan CH , Chang SY , Cheah YL . Laparoscopic removal of intrahepatic foreign body: a novel technique for Management of an unusual Cause of liver abscess--fish bone migration . J Laparoendosc Adv Surg Tech A. 2016 ; 26 : 47 – 50 .
Venkatesan S , Falhammar H . Pyogenic hepatic abscess secondary to gastric perforation caused by an ingested fish bone . Med J Aust. 2019 ; 211 : 451 – e1 .
Venkatesh SH , Sanamandra SK . Large hepatic abscess caused by fish bone . Saudi Med J. 2015 ; 36 : 878 – 9 .
Xiao L , Li JW , Zheng SG . Laparoscopic extraction of a hepatic fish bone mimicking a liver mass after gastric perforation . Dig Dis Sci. 2015 ; 60 : 2538 – 40 .
Yang CY , Kao JH , Liu KL , Chen SJ . Medical treatment of fish bone-related liver abscess . Clin Infect Dis. 2005 ; 41 : 1689 – 90 .
Yen HH , Hsu YC . Education and imaging: gastrointestinal: pyogenic liver abscess associated with a penetrating fish bone . J Gastroenterol Hepatol. 2010 ; 25 : 1900 .
Yu W , Yu H , Ling J , Du J , Yin Z , Li C , et al. Hepatic abscess secondary to stomach perforation by a fish bone: a rare cause of hepatic abscess . Ann Hepatol. 2018 ; 17 : 880 – 3 .
- inflammatory markers
- computed tomography
- epigastric pain
- pathologic fistula
- gastrostomy
- hepatic abscess
- foreign bodies
- laparoscopy
- radio communications
Email alerts
Citing articles via.
- X (formerly Twitter)
Affiliations
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Liver abscess secondary to fishbone ingestion: case report and review of the literature
Niamh grayson, hiba shanti, ameet g patel.
- Author information
- Article notes
- Copyright and License information
Correspondence address. King’s College Hospital, Denmark Hill, London SE5 9RS, UK. Tel: +44-7740-705060; Email: [email protected]
Received 2021 Dec 2; Accepted 2022 Jan 15; Collection date 2022 Feb.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted reuse, distribution, and reproduction in any medium, provided the original work is properly cited.
We report a rare silent migration of a fishbone into the liver and review the relevant literature. A 56-year-old man presented with a 2-day history of dull epigastric pain and raised inflammatory markers. Computerized tomography scan revealed a 4-cm abscess in the left lobe of the liver, with a linear radio-dense foreign body within the collection. At laparoscopy the hepatogastric fistula was disconnected. The fishbone was retrieved from the liver. Gastrostomy was closed with an omental patch. The patient had an uneventful recovery. Fifty-two cases of liver abscess secondary to enterohepatic fishbone migration were reported with over two-thirds presenting with a left-lobe abscess. There was marked variability in the management of liver abscess in the setting of fishbone migration-summarized in table. We believe that laparoscopic drainage of the abscess and extraction of the foreign body offer control of the source of sepsis and diminishes recurrence, whilst having a low-risk profile.
INTRODUCTION
Foreign body ingestion is a common occurrence, majority of these pass without complications [ 1 ]. An estimated 1% of ingested foreign bodies result in gastrointestinal perforation, these are often sharp objects, such as accidentally ingested fishbones [ 2 ]. The sites of perforation vary, with the rectosigmoid or ileocolic being the most common [ 3 ].
We report a rare case of fishbone migration resulting in liver abscess and review of the literature. This was originally described in 1898 by Lambert [ 4 ].
CASE PRESENTATION
A 56-year-old man presented with a 2-day history of epigastric pain, leucocytosis and raised C Reactive Protein (CRP). A computed tomography (CT) scan revealed evidence of a 4.2 × 2.5 cm abscess in the left lobe of the liver (Segment III), with a linear radio-dense foreign body seen within the collection ( Fig. 1 ). There was fat stranding around the pylorus. The patient was treated with antibiotics in his local hospital and a trial of aspiration revealed purulent fluid. An oesphagoduodenoscopy (OGD) was normal with no evidence of foreign body or inflammation in the stomach.
CT scan showing left lobe liver abscess with fishbone.
The patient was transferred to our Hepatopancreaticobiliary (HPB) unit. On arrival, he was clinically well and asymptomatic. A repeat CT scan showed a persistent collection in the liver. On further enquiry, the patient revealed that a few weeks earlier as he had a transient episode of choking and discomfort whilst eating fish.
On laparoscopy, the left lateral segment of the liver was adherent to the gastric antrum ( Fig. 2 ). Adhesions between the liver and stomach were divided with blunt and sharp dissection. The fishbone was pulled out of the liver intact and extracted through the port. The abscess was opened, drained and washed. A sealed fistulous tract was identified at the antrum; this was repaired with an omental patch. The patient had an uneventful recovery and was discharged the following day.
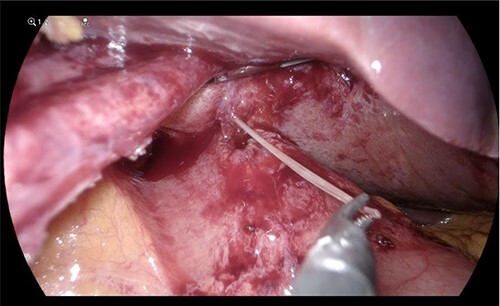
Fishbone extraction from the liver.
Fifty-two cases of liver abscess secondary to enterohepatic fishbone migration have been reported in the English literature ( Table 1 ). Most common symptoms included: anorexia, epigastric pain and fever. The lack of history of ingestion of a fishbone often leads to a diagnostic dilemma. CT scan was diagnostic in 47 that had axial imaging, three fishbones were found intra-operatively and two on autopsy. Over two-thirds of reported cases presented with a left lobe abscess, this is attributable to the anatomical proximity of the stomach.
Review of literature reported cases of enterohepatic fishbone migration
There was marked variability in the management of liver abscess in the setting of fishbone migration. A variety of approaches including laparotomy, laparoscopy, CT guidance and liver resection were utilized to remove the fishbones. Percutaneous drainage usually results in the resolution of liver abscess, but recurrence is likely. Nine patients had the fishbone left in situ , one patient ultimately required a laparotomy for fishbone removal [ 5 ]. There were two mortalities in these patients with the fishbone left in situ (2/7, 29%), these were secondary to overwhelming sepsis, and the fishbones were discovered at autopsy [ 6 , 7 ].
LEARNING POINTS/TAKE-HOME MESSAGES
Left lobe liver abscess should raise the suspicion of a foreign body. Antibiotic treatment and drainage are effective in the short term. The retained foreign body acts as a nidus for recurrent infection and requires removal to prevent recurrence and mortality.
Previous presentation: Poster presentation in UGI conference 2021.
CONFLICT OF INTEREST STATEMENT
None declared.
Kings College London (JISC affiliated).
- 1. Abel RM, Fischer JE, Hendren WH. Penetration of the alimentary tract by a foreign body with migration to the liver. Arch Surg. 1971;102:227–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Horii K, Yamazaki O, Matsuyama M, Higaki I, Kawai S, Sakaue Y. Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case. Surg Today. 1999;29:922–6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. McCanse DE, Kurchin A, Hinshaw JR. Gastrointestinal foreign bodies. Am J Surg. 1981;142:335–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Lambert A. Abscess of the liver of unusual origin. NY Med J. 1898;177–8. [ Google Scholar ]
- 5. Masoodi I, Alsayari K, Al Mohaimeed K, Ahmad S, Almtawa A, Alomair A, et al. . Fish bone migration: an unusual cause of liver abscess. BMJ Case Rep. 2012;2012:bcr0920114838. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. De la Vega M, Rivero JC, Ruiz L, Suarez S. A fish bone in the liver. Lancet. 2001;358:982. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Theodoropoulou A, Roussomoustakaki M, Michalodimitrakis MN, Kanaki C, Kouroumalis EA. Fatal hepatic abscess caused by a fish bone. Lancet. 2002;359:977. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Akhondi H, Sabih DE. Liver Abscess. Treasure Island (FL): StatPearls, 2021. [ Google Scholar ]
- 9. Allam M, Pericleous S. Migrated fish bone induced liver abscess: medical management. Pan Afr Med J. 2020;36:140. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Bandeira-de-Mello RG, Bondar G, Schneider E, Wiener-Stensmann IC, Gressler JB, Kruel CRP. Pyogenic liver abscess secondary to foreign body (fish bone) treated by laparoscopy: a case report. Ann Hepatol. 2018;17:169–73. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Barkai O, Kluger Y, Ben-Ishay O. Laparoscopic retrieval of a fishbone migrating from the stomach causing a liver abscess: report of case and literature review. J Minim Access Surg. 2020;16:418–20. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Beckers G, Magema JP, Poncelet V, Nita T. Successful laparoscopic management of a hepatic abscess caused by a fish bone. Acta Chir Belg. 2021;121:135–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Bekki T, Fujikuni N, Tanabe K, Amano H, Noriyuki T, Nakahara M. Liver abscess caused by fish bone perforation of stomach wall treated by laparoscopic surgery: a case report. Surg Case Rep. 2019;5:79. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Burkholder R, Samant H. Management of fish bone-induced liver abscess with foreign body left in situ. Case Reports Hepatol. 2019;2019:9075198. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Chen J, Wang C, Zhuo J, Wen X, Ling Q, Liu Z, et al. . Laparoscopic management of enterohepatic migrated fish bone mimicking liver neoplasm: a case report and literature review. Medicine (Baltimore). 2019;98:e14705. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Clarencon F, Scatton O, Bruguiere E, Silvera S, Afanou G, Soubrane O, et al. . Recurrent liver abscess secondary to ingested fish bone migration: report of a case. Surg Today. 2008;38:572–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Dangoisse C, Laterre PF. Tracking the foreign body, a rare cause of hepatic abscess. BMC Gastroenterol. 2014;14:167. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Dias AR, Szor DJ, Ferreira CBA, Navarro CL. Uncommon cause of liver abscess. Clin Case Rep. 2018;6:1649–50. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Ede C, Sobnach S, Kahn D, Bhyat A. Enterohepatic migration of fish bone resulting in liver abscess. Case Rep Surg. 2015;2015:238342. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Esseghaier S, Nassej O, Haouas N, Benhassen I, Maamar AB, Daghfous MH. Liver abscess caused by migration of an ingested foreign body. Presse Med. 2015;44:851–3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Fujiwara Y, Shiba H, Nakabayashi Y, Otsuka M, Yanaga K. Hepatic abscess in the Spiegel lobe caused by foreign body penetration: report of a case report. Surg Case Rep. 2017;3:24. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Gaba RC, Bui JT, Carroll RE. Catch of the day: forceps removal of embedded fish bone. J Vasc Interv Radiol. 2013;24:1545. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Goh BK, Yong WS, Yeo AW. Pancreatic and hepatic abscess secondary to fish bone perforation of the duodenum. Dig Dis Sci. 2005;50:1103–6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Gomez Portilla A, Ezurmendia B, Martin E, Lopez de Heredia E, Muriel LJ. Fish bone-related intrahepatic abscess. An underdiagnosed condition? Cir Esp (Engl Ed). 2019;97:116–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Goyal P, Gupta S, Sapire J. Bone causing abdominal groans. J Emerg Med. 2019;57:e95–e7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Hernandez-Villafranca S, Qian-Zhang S, Garcia-Olmo D, Villarejo-Campos P. Liver abscess due to a fish bone injury: a case report and review of the literature. Cir Cir. 2020;88:1–4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Jarry J, Nguyen V, Stoltz A, Imperato M, Michel P. A fish bone-related hepatic abscess. Clin Pract. 2011;1:e115. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Kadowaki Y, Tamura R, Okamoto T, Mori T, Mori T. Ruptured hepatic abscess caused by fish bone penetration of the duodenal wall: report of a case. Surg Today. 2007;37:1018–21. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Kosar MN, Oruk I, Yazicioglu MB, Erol C, Cabuk B. Successful treatment of a hepatic abscess formed secondary to fish bone penetration by laparoscopic removal of the foreign body: report of a case. Ulus Travma Acil Cerrahi Derg. 2014;20:392–4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Lau CW, Wong KM, Gogna A. Image-guided percutaneous transhepatic removal of fish bone from liver abscess. J Radiol Case Rep. 2017;11:1–7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Lee KF, Chu W, Wong SW, Lai PB. Hepatic abscess secondary to foreign body perforation of the stomach. Asian J Surg. 2005;28:297–300. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Li J, Zhao D, Lei L, Zhang L, Yu Y, Chen Q. Liver abscess caused by ingestion of fishbone: a case report. Medicine (Baltimore). 2019;98:e16835. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Liang H, Liu OQ, Ai XB, Zhu DQ, Liu JL, Wang A, et al. . Recurrent upper quadrant pain: a fish bone secondary to gastric perforation and liver abscess. Case Rep Gastroenterol. 2011;5:663–6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Mateus JE, Silva C, Beirao S, Pimentel J. Hepatic abscess induced by fish bone migration: two case reports. Acta Med Port. 2018;31:276–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Matrella F, Lhuaire M, Piardi T, Dokmak S, Bruno O, Maestraggi Q, et al. . Liver hilar abscesses secondary to gastrointestinal perforation by ingested fish bones: surgical management of two cases. Hepatobiliary Surg Nutr. 2014;3:156–62. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Ng CT, Htoo A, Tan SY. Fish bone-induced hepatic abscess: medical treatment. Singapore Med J. 2011;52:e56–8. [ PubMed ] [ Google Scholar ]
- 37. Panebianco A, Lozito RC, Prestera A, Ialongo P, Volpi A, Carbotta G, et al. . Unusual liver abscess secondary to ingested foreign body: laparoscopic management. G Chir. 2015;36:74–5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. Peixoto A, Goncalves R, Macedo G. Liver abscess associated sepsis caused by fish bone ingestion. GE Port J Gastroenterol. 2016;23:322–3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Perera MT, Wijesuriya SR, Kumarage SK, Ariyaratne MH, Deen KI. Inflammatory pseudotumour of the liver caused by a migrated fish bone. Ceylon Med J. 2007;52:141–2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Queiroz RM, Filho FB. Liver abscess due to fish bone ingestion. Pan Afr Med J. 2019;32:26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Santos SA, Alberto SC, Cruz E, Pires E, Figueira T, Coimbra E, et al. . Hepatic abscess induced by foreign body: case report and literature review. World J Gastroenterol. 2007;13:1466–70. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Sim GG, Sheth SK. Retained foreign body causing a liver abscess. Case Rep Emerg Med. 2019;2019:4259646. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Tan CH, Chang SY, Cheah YL. Laparoscopic removal of intrahepatic foreign body: a novel technique for Management of an unusual Cause of liver abscess--fish bone migration. J Laparoendosc Adv Surg Tech A. 2016;26:47–50. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Venkatesan S, Falhammar H. Pyogenic hepatic abscess secondary to gastric perforation caused by an ingested fish bone. Med J Aust. 2019;211:451–e1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Venkatesh SH, Sanamandra SK. Large hepatic abscess caused by fish bone. Saudi Med J. 2015;36:878–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Xiao L, Li JW, Zheng SG. Laparoscopic extraction of a hepatic fish bone mimicking a liver mass after gastric perforation. Dig Dis Sci. 2015;60:2538–40. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Yang CY, Kao JH, Liu KL, Chen SJ. Medical treatment of fish bone-related liver abscess. Clin Infect Dis. 2005;41:1689–90. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Yen HH, Hsu YC. Education and imaging: gastrointestinal: pyogenic liver abscess associated with a penetrating fish bone. J Gastroenterol Hepatol. 2010;25:1900. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Yu W, Yu H, Ling J, Du J, Yin Z, Li C, et al. . Hepatic abscess secondary to stomach perforation by a fish bone: a rare cause of hepatic abscess. Ann Hepatol. 2018;17:880–3. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (356.9 KB)
- Collections

Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Case report
- Open access
- Published: 31 March 2023
Lactococcus lactis endocarditis and liver abscess in an immunocompetent patient: a case report and review of the literature
- Wahib Lahlou ORCID: orcid.org/0000-0003-4618-8865 1 na1 ,
- Abderrahim Bourial ORCID: orcid.org/0000-0003-3801-1162 4 na1 ,
- Taib Maaouni 1 ,
- Ahmed Bensaad ORCID: orcid.org/0000-0001-6718-1588 2 ,
- Ilham Bensahi ORCID: orcid.org/0000-0003-3540-5043 3 ,
- Mohamed Sabry 3 &
- Mohamed Miguil 1
Journal of Medical Case Reports volume 17 , Article number: 115 ( 2023 ) Cite this article
2953 Accesses
5 Citations
Metrics details
Over the last two decades, several cases of infections caused by Lactococcus lactis have been reported. This Gram-positive coccus is considered non-pathogenic for humans. However, in some rare cases, it can cause serious infections such as endocarditis, peritonitis, and intra-abdominal infections.
Case presentation
A 56-year-old Moroccan patient was admitted to the hospital because of diffuse abdominal pain and fever. The patient had no past medical history. Five days before his admission, he developed abdominal pain in the right lower quadrant along with chills and feverish sensations. Investigations showed a liver abscess, which was drained, and the microbiological study of the pus revealed Lactococcus lactis subsp. cremoris . Three days after admission, control computed tomography objectified splenic infarctions. Cardiac explorations were performed and showed a floating vegetation on the ventricle side of the aortic valve. We retained the diagnosis of infectious endocarditis according to the modified Duke criteria. The patient was declared afebrile on day 5 and the evolution was clinically and biologically favorable. Lactococcus lactis subsp. cremoris , formerly known as Streptococcus cremoris , is a rare cause of human infections. The first case of Lactococcus lactis cremoris endocarditis was reported in 1955. This organism includes three subspecies: lactis , cremoris , and hordniae . A MEDLINE and Scopus search showed only 13 cases of infectious endocarditis due to Lactococcus lactis , with subsp. cremoris identified in four of the cases.
Conclusions
To our knowledge, this is the first case report of the co-occurrence of Lactococcus lactis endocarditis and liver abscess. Despite its reported low virulence and good response to antibiotic treatment, Lactococcus lactis endocarditis must be considered a serious disease. It is imperative for a clinician to suspect this microorganism of causing endocarditis when they notice signs of infectious endocarditis in a patient with a history of consumption of unpasteurized dairy products or contact with farm animals. The finding of a liver abscess should lead to an investigation of endocarditis, even in previously healthy patients without obvious clinical signs of endocarditis.
Peer Review reports
Over the last two decades, several cases of infections caused by Lactococcus lactis have been reported. Widely used for the production of fermented products, this Gram-positive coccus is considered nonpathogenic for humans [ 1 ]. However, in some rare cases involving both immunocompetent and immunocompromised patients [ 2 ], it can cause serious infections such as endocarditis, peritonitis, and intra-abdominal infections[ 3 ].
In this article, we report a rare case of an immunocompetent 56-year-old male with a history of raw milk consumption who presented with a Lactococcus -associated liver abscess and endocarditis.
To our knowledge, this is the first reported case in the literature (on the basis of the MEDLINE and Scopus databases) of a concurrent discovery of the association of a liver abscess and an endocarditis caused by Lactococcus lactis .
A 56-year-old Moroccan patient was admitted to the hospital for diffuse abdominal pain and fever. The patient was a bricklayer, reported no past medical history and no alcohol consumption, but was an active smoker. Five days before admission, the patient developed abdominal pain in the right lower quadrant along with chills and feverish sensations. Initially, the patient received symptomatic treatment with phloroglucinol (80 mg three times a day) and showed no improvement. In contrast, his abdominal pain increased and became diffuse.
On admission, his temperature was 39 °C, his pulse was 126 beats per minute, his blood pressure was 140/76 mmHg, his respiratory rate was 15 breaths per minute, his oxygen saturation was 94% in ambient air, and his Glasgow Coma Scale (GCS) score was 15/15.
Physical examination showed diffuse abdominal tenderness on palpation and decreased vesicular murmurs in the right chest. There were no valvular murmurs, and no mucocutaneous lesions of infectious endocarditis such as Janeway lesions, Osler nodes, or splinter hemorrhages under the fingernails. The rest of the examination was normal.
The biological assessment, carried out in the emergency department, showed leucocytosis with neutrophilia, hypereosinophilia, and monocytosis (white blood cell count of 14,960 per mm 3 , neutrophil count of 9930 per mm 3 , eosinophil count of 2570 per mm 3 , and monocyte count of 1210 per mm 3 ). The plasma C-reactive protein level was 419.37 mg/l, and the procalcitonin level was 4.660 ng/ml. The liver function tests were elevated, with an aspartate aminotransferase level of 139.1 UI/L and an alanine aminotransferase level of 279 UI/L. Kidney function was normal with a creatinine level of 8.7 mg/L and urea level of 0.52 g/L. The electrocardiogram performed on admission was normal.
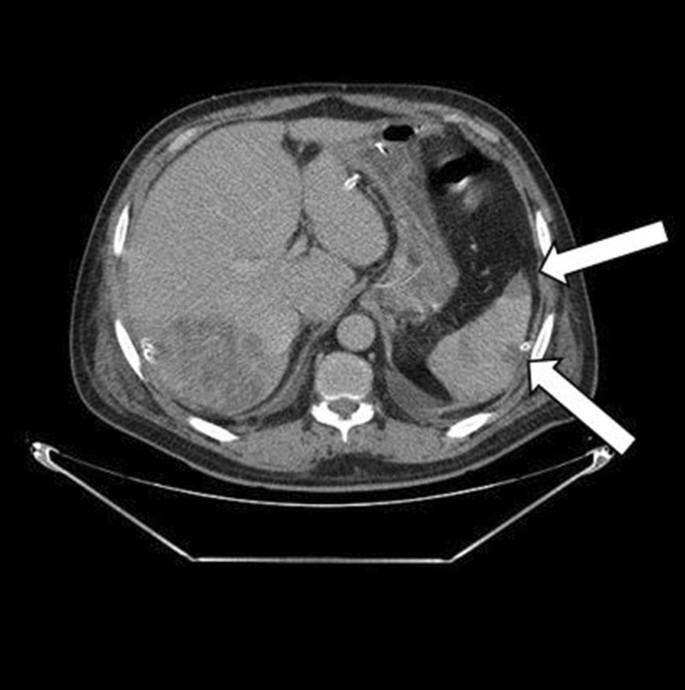
Thoraco-abdomino-pelvic computed tomography (CT) showed right basal pneumonia, mild bilateral pleural effusion, low abundance perihepatic fluid effusion, and an abscess in segment VII of the liver measuring 87 × 70 mm. (Figs . 1 and 2 ).
Abdominal computed tomography revealed a multiloculated hypodensity in segment VII, suggesting a liver abscess (white arrowhead)
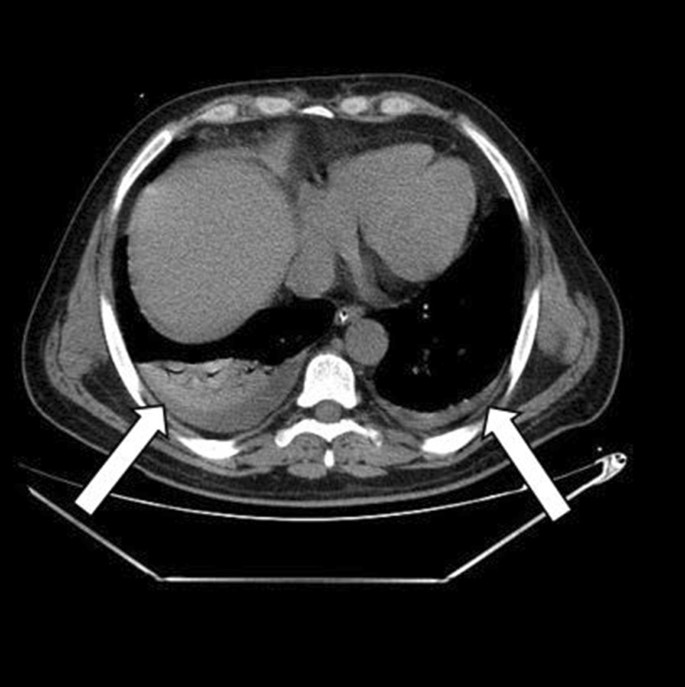
Thoracic computed tomography revealed a mild predominantly right bilateral pleural effusion (white arrowheads)
Surgical drainage was recommended and performed under general anesthesia. The exploration showed a fissured abscess through which we noted the exit of pus. It was drained by a Salem sump drain with pus sampling for cytobacteriological study. The pus was cultured and grew Lactococcus lactis subsp. cremoris . During hospitalization, repeated aerobic and anaerobic blood cultures were taken and cultured, all of which were negative.
The postoperative follow-up was simple. The patient was treated empirically with intravenous antibiotics: metronidazole (500 mg three times daily), imipenem (500 mg four times daily), and amikacin (1 g once a day). The amikacin was stopped at day 5. Three days after admission, we carried out a control CT that objectified a more organized aspect of the pre-suppurative phase liver abscesses and areas of splenic infarction (Fig. 3 ). Transthoracic echocardiography was performed and was normal with no evidence of vegetations, no valvular or paravalvular regurgitation, and no aortic abscess or pericardial effusion. A decision to carry out transesophageal echocardiography was made, where a floating vegetation on the ventricle side of the aortic valve measuring 8 × 5 mm was observed and there were no imaging of an abscess or Valsalva aneurysm (Fig. 4 ).
Control abdominal computed tomography revealed areas of splenic infarction (white arrowheads)
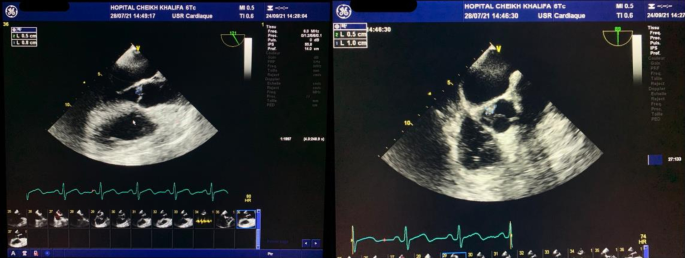
Transesophageal echocardiography showed a floating and vibratile vegetation measuring 8 × 5 mm on the ventricular side of the aortic valve
Investigations of immune function demonstrated that he was HIV negative.
The patient was declared afebrile on day 5. The drainage catheter was removed on day 6 when the drained fluid was minimal.
As part of the endocarditis extension assessment, the patient underwent a cerebral CT that showed no abnormalities.
In total, the patient was treated with imipenem for 4 weeks and metronidazole was also continued for 3 weeks to cover other potential anaerobic germs.
The outcome was clinically and biologically favorable with negativation of the infection’s biomarkers (procalcitonin, C-reactive protein, and total white blood cell count) without occurrence of AV-type electrical complications.
On follow-up in the outpatient clinic after 2 months, the patient was well and asymptomatic with normalized biochemistry and almost complete regression of the liver abscess and splenic infarctions on CT (Fig. 5 ). Moreover, on the control transesophageal echocardiography, we remarked that the vegetation had decreased in size without the occurrence of any complications.
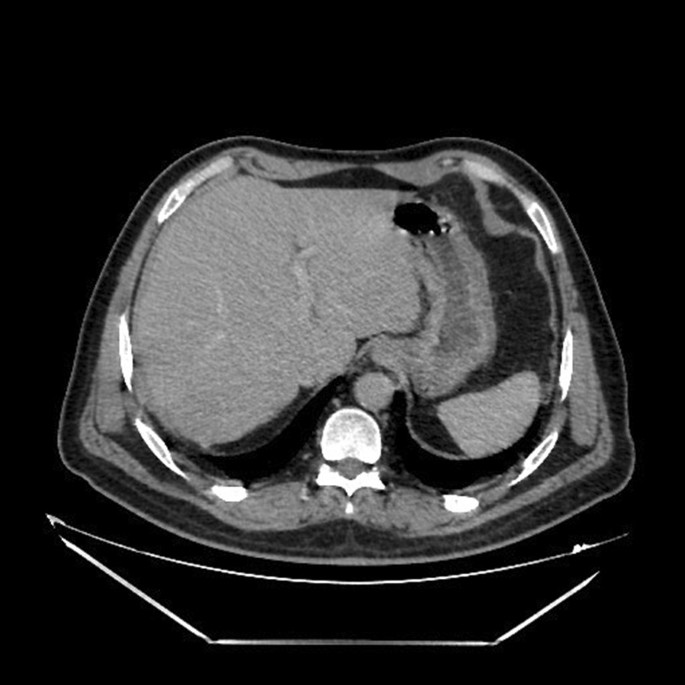
Control computed tomography on follow-up after 2 months showed almost complete regression of the liver abscess and splenic infarctions
The patient was reviewed in consultation after 8 months, and was totally asymptomatic.
Discussion and conclusions
To our knowledge, and up to date in the current literature, this is the first described case of concurrent discovery of a liver abscess associated with endocarditis caused by Lactococcus lactis.
Lactococcus lactis is a Gram-positive bacterium used for the production of fermented dairy products, particularly cheddar cheese. Five species of the genus Lactococcus have been described: L. lactis , L. garvieae , L. piscium , L. plantarum , and L. raffinolactis [ 4 , 5 ].
L. lactis actually includes three subspecies: L. lactis subsp. lactis , L. lactis subsp. cremoris , and L. lactis subsp. hordniae [ 4 , 5 ].
Most bacteria employed in food preparation are killed during digestion (following ingestion), but it has been established that Lactococcus remains viable after transit through the gastrointestinal tract, which is considered to be the mechanism of Lactococcus lactis infection in humans, especially when there is a loss of intestinal wall integrity[ 2 , 6 ]. This may justify colonoscopy as part of the investigation.
In some cases (similar to ours), the ingestion of unpasteurized milk, sour cream, or yogurt was recognized. However, in other cases, there was no history of ingestion of unpasteurized dairy products. Owing to the rarity of Lactococcus lactis infection, the source of this infection has not been well demonstrated. The hypotheses regarding the source of infection include the ingestion of unpasteurized dairy products or direct intraluminal inoculation from contaminated hands[ 7 ].
Lactococcus lactis has low virulence and is considered nonpathogenic. However, it has recently been considered an opportunistic pathogen microbe. A pathophysiological mechanism has been described to explain the virulence of this microorganism in the genesis of infectious endocarditis. Indeed, a study carried out in 2016 showed that Lactococcus lactis expresses the glycoprotein Cnm, which promotes its adhesion to type I collagen and to cardiac tissues (in particular the tissues of the aortic valve) [ 8 ].
We retained the diagnosis of infectious endocarditis for our patient according to the modified Duke criteria. [ 9 , 10 ]. Repeated blood cultures taken during hospitalization did not grow any specific pathogen that could probably be attributed to previous antibiotic treatment. According to the literature, the rate of culture-negative endocarditis varies from 2.1% to 35% [ 11 ]. In our case, the vegetation was not visualized on transthoracic echocardiography although it was a quite voluminous aortic localization and this imaging had good sensitivity for the exploration of the aortic sigmoids [ 12 ]. This highlights the fact that it is necessary to perform transesophageal echocardiography when endocarditis is a clinical possibility.
Infectious endocarditis due to Lactococcus lactis is very rare, and a MEDLINE and Scopus search (Table 1 ) identified only 13 cases of infectious endocarditis due to Lactococcus lactis , with the subsp. cremoris identified in four of the cases. In these four cases, including ours, the affected valve was the aortic valve. However, in other cases, endocarditis affected the mitral valve, which is the most commonly involved valve, followed by the tricuspid valve. The outcomes of the few reported cases were good: only two patients died (including one infant diagnosed postmortem and one adult whose course was complicated by bilateral uncal herniation due to multiple intracerebral hemorrhages). This underlines the good prognosis of Lactococcus lactis endocarditis.
Liver abscess is the second most common localization of Lactococcus lactis infections after endocarditis. Reviewing the MEDLINE and Scopus databases, we found nine cases of hepatic abscess due to Lactococcus lactis : most frequently Lactococcus lactis subsp. cremoris in four cases, Lactococcus lactis subsp. lactis in one case, and no available data regarding the subspecies in four cases [ 1 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 ].
We remark that six out of the nine cases did not accomplish proper cardiac exploration (transthoracic echocardiography nor transesophageal echocardiography). Note that in the other three cases, no available data were found.
Our case is the first liver abscess described in the literature with a proper cardiac exploration that found a co-occurrence of infectious endocarditis. We therefore wonder if this association is underdiagnosed as opposed to what is described, and find it logical to recommend systematic ultrasound cardiac exploration in the case of any Lactococcus lactis hepatic abscess.
A liver abscess formation is explained by its anatomical and physiological singularity. The liver receives blood from the systemic and portal circulations, from which the infected bloodstream can carry the bacterium, and the infection spread in this case was considered hematogenous. The usual pathophysiology behind liver abscess formation can be assumed as bowel content leakage and peritonitis rout. The bacteria can travel through the portal vein to reach the liver and reside there. Less frequently, the infection can originate from the biliary system[ 32 ].
Table 2 presents all available multiple localizations of Lactococcus lactis infections. Nine cases have been described in the literature, from which we find four cases of endocarditis and five liver abscesses as the starting point of the systemic infection.
Six out of the nine cases indicated Lactococcus lactis subsp. cremoris , knowing that the other three cases lacked information and did not specify the subspecies of Lactococcus lactis . Therefore, the cremoris subspecies is more likely to be spread systemically and carried to multiple organs, regardless of the infection starting point, as this hypothesis is consistent with our case.
We found that consumption of unpasteurized milk or cheese was present in three out of the nine cases. It is plausible that the inoculation of the microorganism occurred through an orofecal mechanism. Although Lactococcus inoculation is more prone to be accomplished through the digestive duct, endocarditis and liver abscess seem to be equally frequent as a triggering systemic infection site.
Underlying conditions were documented in eight out of the nine cases identified in the MEDLINE and Scopus database articles and only one patient had an immunocompromised state related to his condition (cholangiocarcinoma). On the basis of the literature, immunodeficiency or immunocompromisation may be a predisposing factor linked with Lactococcus lactis infection with liver abscess localization[ 3 ].
The most frequent localizations that lead to multiple localizations infection other than the heart and the hepatobiliary tract are the pleura, lungs, brain, retroperitoneal organs, bones, and so on, as they are often the starting infection sites. [ 3 ]
The majority of hepatobiliary-starting Lactococcus infection cases did not benefit from proper cardiac exploration. We found that cases 2, 6, and 9 had positive blood culture with a non-specific endocarditis germ (minor modified Duke criteria) with some other minor criterion. On the basis of the modified Duke criteria, these cases had a score of 3, compatible with a possible endocarditis diagnosis. We therefore propose a systematic ultrasound cardiac exploration in front of any Lactococcus lactis hepatic abscess or multiple localization Lactococcus lactis infection, looking for an endocarditis echocardiographic finding.
Pleural effusion, especially in the right chest, was frequently linked with Lactococcus lactis infections, particularly when the infection started with liver abscesses. The possible mechanism of propagation might be through the bloodstream, as well as through a locoregional process, considering the anatomical links.
The outcome was favorable in the majority of cases, suggesting that early treatment may be a major prognostic factor in this kind of infection.
One of the interesting findings in this case was the elevated monocyte count. This patient presented concomitant monocytosis within the endocarditis episode. It is known that monocytosis can be caused by a wide variety of neoplastic and nonneoplastic conditions [ 33 ]. The various causes of monocytosis can be divided into two broad categories: clonal or reactive, from which acute infections such as endocarditis can be an etiologic factor [ 34 ]. Infective-endocarditis-related bacteria are described in the literature as activating factors of blood monocytes. Activated monocytes are believed to be important factors, participating in the formation of endocarditis vegetations by producing cytokines and procoagulant factors that enhance the development of the infected coagulum, formally known as vegetation [ 35 , 36 ].
Lactococcus lactis , formerly known to be a nonpathogenic microorganism, has contributed to several cases of human infections, including infectious endocarditis and liver abscesses. It is essential for a clinician to suspect this microorganism of causing endocarditis when they notice signs of infectious endocarditis in a patient with a history of consumption of unpasteurized dairy products or contact with farm animals. This case suggests the hypothesis that the finding of a liver abscess may require an investigation of endocarditis even in previously healthy patients without obvious clinical signs of endocarditis.
Here, we report here the fourteenth case of endocarditis caused by Lactococcus lactis described in the literature and the first case report of the co-occurrence of Lactococcus lactis endocarditis and liver abscess.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Computed tomography
Human immunodeficiency virus
- Lactococcus lactis
Lactococcus garvieae
Lactococcus piscium
Lactococcus plantarum
Lactococcus rafinolactis
Antolín J, Cigüenza R, Salueña I, Vázquez E, Hernández J, Espinós D. Liver abscess caused by Lactococcus lactis cremoris: a new pathogen. Scand J Infect Dis. 2004;36:490–1.
Article PubMed Google Scholar
Drouault S, Corthier G, Ehrlich SD, Renault P. Survival, physiology, and lysis of Lactococcus lactis in the digestive tract. Appl Environ Microbiol. 1999;65:4881–6.
Article CAS PubMed PubMed Central Google Scholar
Shimizu A, Hase R, Suzuki D, Toguchi A, Otsuka Y, Hirata N, et al . Lactococcus lactis cholangitis and bacteremia identified by MALDI-TOF mass spectrometry: a case report and review of the literature on Lactococcus lactis infection. J Infect Chemother. 2019;25:141–6.
Song AA-L, In LLA, Lim SHE, Rahim RA. A review on Lactococcus lactis : from food to factory. Microb Cell Factories. 2017;16:55.
Article Google Scholar
Parapouli M, Delbès-Paus C, Kakouri A, Koukkou A-I, Montel M-C, Samelis J. Characterization of a wild, novel nisin A-producing Lactococcus strain with an L. lactis subsp. cremoris genotype and an L. lactis subsp. lactis phenotype, isolated from Greek raw milk. Appl Environ Microbiol. 2013;79:3476–84.
Rostagno C, Pecile P, Stefàno PL. Early Lactococcus lactis endocarditis after mitral valve repair: a case report and literature review. Infection. 2013;41:897–9.
Article CAS PubMed Google Scholar
Georgountzos G, Michopoulos C, Grivokostopoulos C, Kolosaka M, Vlassopoulou N, Lekkou A. Infective endocarditis in a young adult due to Lactococcus lactis : a case report and review of the literature. Case Rep Med. 2018;2018: e5091456.
Freires IA, Avilés-Reyes A, Kitten T, Simpson-Haidaris PJ, Swartz M, Knight PA, et al . Heterologous expression of Streptococcus mutans Cnm in Lactococcus lactis promotes intracellular invasion, adhesion to human cardiac tissues and virulence. Virulence. 2017;8:18–29.
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F, et al . 2015 ESC Guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075–128.
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG, Ryan T, et al . Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–8.
Subedi S, Jennings Z, Chen SC-A. Laboratory approach to the diagnosis of culture-negative infective endocarditis. Heart Lung Circ. 2017;26:763–71.
Reynolds HR, Jagen MA, Tunick PA, Kronzon I. Sensitivity of transthoracic versus transesophageal echocardiography for the detection of native valve vegetations in the modern era. J Am Soc Echocardiogr. 2003;16:67–70.
Wood HF, Jacobs K, McCarty M. Streptococcus lactis isolated from a patient with subacute bacterial endocarditis. Am J Med. 1955;18:345–7.
Mannion PT, Rothburn MM. Diagnosis of bacterial endocarditis caused by Streptococcus lactis and assisted by immunoblotting of serum antibodies. J Infect. 1990;21:317–8.
Pellizzer G, Benedetti P, Biavasco F, Manfrin V, Franzetti M, Scagnelli M, et al . Bacterial endocarditis due to Lactococcus lactis subsp. cremoris: case report. Clin Microbiol Infect. 1996;2:230–2.
Halldórsdóttir HD, Haraldsdóttir V, Böđvarsson Á, Þorgeirsson G, Kristjánsson M. Endocarditis caused by Lactococcus cremoris. Scand J Infect Dis. 2002;34:205–6.
Kiss J, Zahár Á, Nyíri P, Prinz G. A case of femoral osteomyelitis caused by Lactococcus. Orv Hetil. 2005;146:613–8.
PubMed Google Scholar
Zechini B, Cipriani P, Papadopoulou S, Di Nucci G, Petrucca A, Teggi A. Endocarditis caused by Lactococcus lactis subsp. lactis in a patient with atrial myxoma: a case report. Diagn Microbiol Infect Dis. 2006;56:325–8.
Resch M, Schichtl T, Endemann DH, Griese DP, Kasprzak P, Djavidani B, et al . General aneurysmatosis due to cheese consumption: complications of an endocarditis caused by Lactococcus cremoris. Int J Cardiol. 2008;126:e8-9.
Lin K-H, Sy CL, Chen C-S, Lee C-H, Lin Y-T, Li J-Y. Infective endocarditis complicated by intracerebral hemorrhage due to Lactococcus lactis subsp. cremoris. Infection. 2010;38:147–9.
Taniguchi K, Nakayama M, Nakahira K, Nakura Y, Kanagawa N, Yanagihara I, et al . Sudden infant death due to Lactococcal infective endocarditis. Leg Med. 2016;19:107–11.
Article CAS Google Scholar
Mansour B, Habib A, Asli N, Geffen Y, Miron D, Elias N. A case of infective endocarditis and pulmonary septic emboli caused by Lactococcus lactis . Case Rep Pediatr. 2016;2016:1–4.
Chen F, Zhang Z, Chen J. Infective endocarditis caused by Lactococcus lactis subsp. lactis and Pediococcus pentosaceus : a case report and literature review. Medicine (Baltimore). 2018;97: e13658.
Nakarai T, Morita K, Nojiri Y, Nei J, Kawamori Y. Liver abscess due to Lactococcus lactis cremoris. Pediatr Int. 2000;42(6):699–701. https://doi.org/10.1046/j.1442-200x.2000.01294.x .
Güz G, Ye ZA. Ailevi Akdeniz Atefli olan bir vakada Lactococcus Lactis’e ikincil portal ven trombozu ve karaci¤er absesi. :4.
Denholm J, Horne K, McMahon J, Grayson ML, Johnson P. Yoghurt consumption and damaged colonic mucosa: a case of Lactococcus lactis liver abscess in an immunocompetent patient. Scand J Infect Dis. 2006;38:739–41.
Imai K, Beppu T, Hayashi H, Masuda T, Mizumoto T, Ishiko T, et al . Two cases of panperitonitis due to intraperitoneal rupture of gas-containing pyogenic liver abscesses. Jpn J Gastroenterol Surg. 2007;40:421–6.
Kim HS, Park DW, Youn YK, Jo YM, Kim JY, Song JY, et al . Liver abscess and empyema due to Lactococcus lactis cremoris. J Korean Med Sci. 2010;25:1669–71.
Article PubMed PubMed Central Google Scholar
Lee JY, Seo MY, Yang J, Kim K, Chang H, Kim SC, et al . Polymicrobial peritonitis with Lactococcus lactis in a peritoneal dialysis patient. Chonnam Med J. 2014;50:67–9.
Fragkiadakis K, Ioannou P, Barbounakis E, Samonis G. Intra-abdominal abscesses by Lactococcus lactis ssp. cremoris in an immunocompetent adult with severe periodontitis and pernicious anemia. IDCases. 2017;7:27–9.
El Hattabi K, Bouali M, Sylvestre K, Bensardi FZ, El Bakouri A, Khalid Z, et al . Lactococcus lactis ssp lactis a rare cause of liver abscesses: a case report and literature review. Int J Surg Case Rep. 2021;81: 105831.
Akhondi H, Sabih DE. Liver abscess. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
Lynch DT, Hall J, Foucar K. How I investigate monocytosis. Int J Lab Hematol. 2018;40:107–14.
Mangaonkar AA, Tande AJ, Bekele DI. Differential diagnosis and workup of monocytosis: a systematic approach to a common hematologic finding. Curr Hematol Malig Rep. 2021;16:267–75.
Veltrop MHAM, Bancsi MJLMF, Bertina RM, Thompson J. Role of monocytes in experimental Staphylococcus aureus endocarditis. Infect Immun. 2000;68:4818–21.
Werdan K, Dietz S, Löffler B, Niemann S, Bushnaq H, Silber R-E, et al . Mechanisms of infective endocarditis: pathogen–host interaction and risk states. Nat Rev Cardiol. 2014;11:35–50.
Download references
Acknowledgements
Not applicable.
Author information
WL and AB contributed equally to the work
Authors and Affiliations
Department of Polyvalent Resuscitation Unit, Cheikh Khalifa International University Hospital, Mohammed VI University of Sciences and Health, Casablanca, Morocco
Wahib Lahlou, Taib Maaouni & Mohamed Miguil
Department of Visceral Surgery, Cheikh Khalifa International University Hospital, Mohammed VI University of Sciences and Health, Casablanca, Morocco
Ahmed Bensaad
Department of Cardiology, Cheikh Khalifa International University Hospital, Mohammed VI University of Sciences and Health, Casablanca, Morocco
Ilham Bensahi & Mohamed Sabry
Cheikh Khalifa International University Hospital, Mohammed VI University of Sciences and Health, Casablanca, Morocco
Abderrahim Bourial
You can also search for this author in PubMed Google Scholar
Contributions
WL, TM, MM, and ABe took part in taking care of the patient. IB and MS performed the echocardiography and assisted in the drafting of the manuscript. ABe took part in researching the bibliography and assisted in the drafting of the manuscript. WL and ABo took part in researching the bibliography and writing the article. TM and MM revised the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Wahib Lahlou .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written informed consent was obtained from the patient for publication of this case report with accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lahlou, W., Bourial, A., Maaouni, T. et al. Lactococcus lactis endocarditis and liver abscess in an immunocompetent patient: a case report and review of the literature. J Med Case Reports 17 , 115 (2023). https://doi.org/10.1186/s13256-022-03676-1
Download citation
Received : 14 June 2022
Accepted : 08 November 2022
Published : 31 March 2023
DOI : https://doi.org/10.1186/s13256-022-03676-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Endocarditis
- Lactococcus lactis subsp. cremoris
- Liver abscess
- Splenic infarction
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
In this case report and review of the literature, we found that fusobacterial liver abscesses resulted in good outcomes with contemporary medical and surgical care. ... Cigarrán S, Neches C, Lamas JM, García-Trio G, Alonso M, Saavedra J. A case report of a pyogenic liver abscess caused by Fusobacterium nucleatum in a patient with autosomal ...
Liver abscess is a rare condition. There are multiple etiologies and mortality linked to the infections or local complications is high. The rapid diagnosis and the implementation of an adequate and effective treatment are essential to allow healing without sequels. ... [Liver abscess : case report and literature review] Rev Med Liege. 2020 Nov ...
This case report and discussion will attempt to review the literature on the etiology, diagnosis and treatment of hepatic abscess for the emergency physician. INTRODUCTION. Hepatic abscesses are a relatively uncommon occurrence in North America. They are seen in approximately 2.3 cases per 100,000 with higher rates found among men than women.
It has been found to be a common cause of liver abscess in Taiwan. However, recently there has been the change in the trend of this infection in the United States . And now it is one of the common causes of PLA in the United States. We present a case of Klebsiella liver abscess with bacteremia.
Background: Fusobacteriae are facultative anaerobic gram-negative bacilli which cause a range of invasive infections, amongst which pyogenic liver abscesses are rare. We describe a case of Fusobacterium nucleatum liver abscess and review the relevant literature. Case presentation: A 51-year-old lady presented with a 4-day history of abdominal pain, diarrhoea, fever, rigors, and lethargy.
Aim: To evaluate the safety and efficacy of the minimally invasive surgical approach (laparoscopic drainage) of liver abscesses in selected cases. Case report: Male, 58 years old, from a rural area, presented with epigastric abdominal pain, fever, weight loss, loss of appetite, a palpable mass in the epigastrium and neutrophilic leukocytosis ...
We report a rare case of fishbone migration resulting in liver abscess and review of the literature. This was originally described in 1898 by Lambert . CASE PRESENTATION. A 56-year-old man presented with a 2-day history of epigastric pain, leucocytosis and raised C Reactive Protein (CRP).
We report a rare silent migration of a fishbone into the liver and review the relevant literature. A 56-year-old man presented with a 2-day history of dull epigastric pain and raised inflammatory markers. Computerized tomography scan revealed a 4-cm abscess in the left lobe of the liver, with a linear radio-dense foreign body within the collection.
HAP is a rare but potentially life-threatening complication of pyogenic or amoebic liver abscesses; if left untreated, HAP can rupture and cause life-threatening bleeding.2 3 Therefore, early detection and therapeutic intervention for even rare complications are important to prevent rupture. Abdominal ultrasonography is not only useful in the diagnosis of liver abscesses but is also necessary ...
Our case is the first liver abscess described in the literature with a proper cardiac exploration that found a co-occurrence of infectious endocarditis. ... Lactococcus lactis ssp lactis a rare cause of liver abscesses: a case report and literature review. Int J Surg Case Rep. 2021;81: 105831.