REVIEW article
Early detection and outcome in borderline personality disorder.

- Department of Neuroscience, University of Turin, Turin, Italy
Borderline personality disorder (BPD) is a severe and heterogeneous mental disorder that is known to have the onset in young age, often in adolescence. For this reason, it is of fundamental importance to identify clinical conditions of childhood and adolescence that present a high risk to evolve in BPD. Investigations indicate that early borderline pathology (before 19 years) predict long-term deficits in functioning, and a higher percentage of these patients continue to present some BPD symptoms up to 20 years. There is a general accordance among investigators that good competence in both childhood and early adulthood is the main predictive factor of excellent recovery in BPD patients. Some authors suggest that specific childhood personality traits can to be considered precursors of adult BPD, as well as some clinical conditions: disruptive behaviours, disturbance in attention and emotional regulation, conduct disorders, substance use disorders, and attention-deficit-hyperactivity disorder. Unfortunately, diagnosis and treatment of BPD is usually delayed, also because some clinicians are reluctant to diagnose BPD in younger individuals. Instead, the early identification of BPD symptoms have important clinical implications in terms of precocious intervention programs, and guarantees that young people with personality disorders obtain appropriate treatments. This review is aimed to collect the current evidences on early risk and protective factors in young people that may predict BPD onset, course, and outcome.

Introduction
Borderline personality disorder (BPD) is a severe and heterogeneous mental disturbance connoted by a pattern of identity diffusion, interpersonal disturbances, and chronic instability, with episodes of severe affective and impulsive dyscontrol ( 1 ). Personality disorders (PD) do not suddenly emerge in the adulthood; in fact, prodromal signs and processes that confer vulnerability to later personality pathology are already present in young age, often in adolescence ( 2 – 5 ). In adolescents, epidemiological data reported a point prevalence around 0.9%, but studies in this age group are still scarce ( 6 ). Cumulative prevalence rates of BPD in youths are respectively 1.4% and 3.2% at 16 years and at 22 years. In mental health setting, the diagnosis of BPD in adolescence reach a prevalence of 11% in psychiatric outpatients and up to 50% in inpatients ( 2 , 6 – 8 ). Investigations indicate that early borderline pathology (before 19 years) predicts long-term deficits in functioning, and a higher percentage of these patients continue to present some BPD symptoms up to 20 years. ( 9 ) A considerable proportion of these individuals continue to suffer from borderline symptoms up to 20 years ( 10 ).
For this reason, clinical conditions of childhood and adolescence that present a high risk to evolve in BPD should be carefully monitored. Unfortunately, diagnosis and treatment of BPD is usually delayed as some symptoms are underestimated and clinician have hesitation to diagnose BPD in younger individuals. Stigma, the incompleteness of personality development in this age group, and similarities between physiological adolescent upheaval and BPD symptoms are the main reasons for this reluctance ( 11 ). Indeed, early identification of BPD symptoms may promote early intervention programs that should guarantee appropriate treatments in young people. Some retrospective studies in adult patients ( 12 , 13 ) showed that the mean age of first psychiatric contact was 17 to 18 years and that the common failure in the diagnosis at first presentation resulted in losing the opportunity to set up early interventions. Several factors, including precocious environmental factors, child and adolescent temperamental characteristics, early psychopathological features, and neurobiological correlates were identified as predictors of early BPD onset. Although the importance of an early diagnosis to improve long-term outcome of the disorder is widely accepted, this issue is not extensively studied and many questions still remain open. In order to improve our knowledge on risk factors in young people that may predict early BPD onset, course, and outcome, we conducted a review to collect and summarize the available evidence in literature.
In October 2018, an electronic search on PubMed about early prodromal factors and precursors of BPD without any filter or MESH restriction was performed, using the following search string: “borderline personality disorder” AND “early symptoms” OR “borderline personality disorder” AND “precursors” OR “borderline personality disorder” AND “prodromal factors” OR “borderline personality disorder” AND “childhood” OR “borderline personality disorder” AND “adolescence” OR “borderline personality disorder” AND “early symptoms” AND “outcome.” This string ensured a high sensitive search for the published works indexed in PubMed. A limitation of this review is that PubMed was the only database used to search the articles. Overlapping studies were excluded. We included the following types of publications: controlled trials, observational studies, longitudinal and prospective studies, cohort studies, and reviews from January 2000 until November 2018. Publications must concern early factors that predict BPD in young age as the main topic. We excluded publications written in a language other than English.
The search described in the previous section provided 2,193 records, and among them 1,788 overlapping studies were excluded. Total records included in the review were 405. Eligibility status for articles was determined in the following way: 1) all studies were screened on the basis of title and abstract; 2) papers that have passed the initial screening were reviewed on the basis of a careful examination of the full manuscript content. Three hundred and four were excluded because they did not fit the objective of the review, 19 because were not written in English, 3 for the lack of the complete manuscript. Thus, this review included 79 records, including 7 reviews, 51 longitudinal/prospective studies, 3 retrospective studies, 1 observational study, 1 commentary/expert article, and 16 controlled trials.
BPD symptoms and diagnosis were assessed with the following evaluation instrument: in the majority of cases for adult was used the official tool of DSM (Structured Clinical Interview for DSM-IV Axis II Personality Disorders SCID-II, and for DSM-5 Personality Disorders SCID-PD). Specifically for children and adolescents, most of the studies adopted the Borderline Personality Features Scale for Children (BPFS-C) ( 14 ) including a newly developed parent report version of the measure (BPFS-P) ( 15 ).
Number of studies participants ranged between 40 and 6,050. Seven studies included only females; one study included only males; 3 studies did not report the gender percentage; the remaining studies had an equal distribution of males and females. The vast majority of patients in the reviewed articles was Caucasian and this is a limitation both in terms of clinical and socio-cultural limitations. Duration of the longitudinal/prospective studies presented a wide range between 1 and 30 years. Ninety percent of studies enrolled participants from the community (40% of these were “high-risk” subjects on the basis of the presence of relevant risk factors, i.e. economic disadvantages), 10% from the clinical settings. Drop-out rates were acceptable, with a retention ranged between 43% and 96%. Majority of studies had a retention ≥70%.
The selection process and a schematic representation of the results are represented in the literature search flowchart ( Figure 1 ).
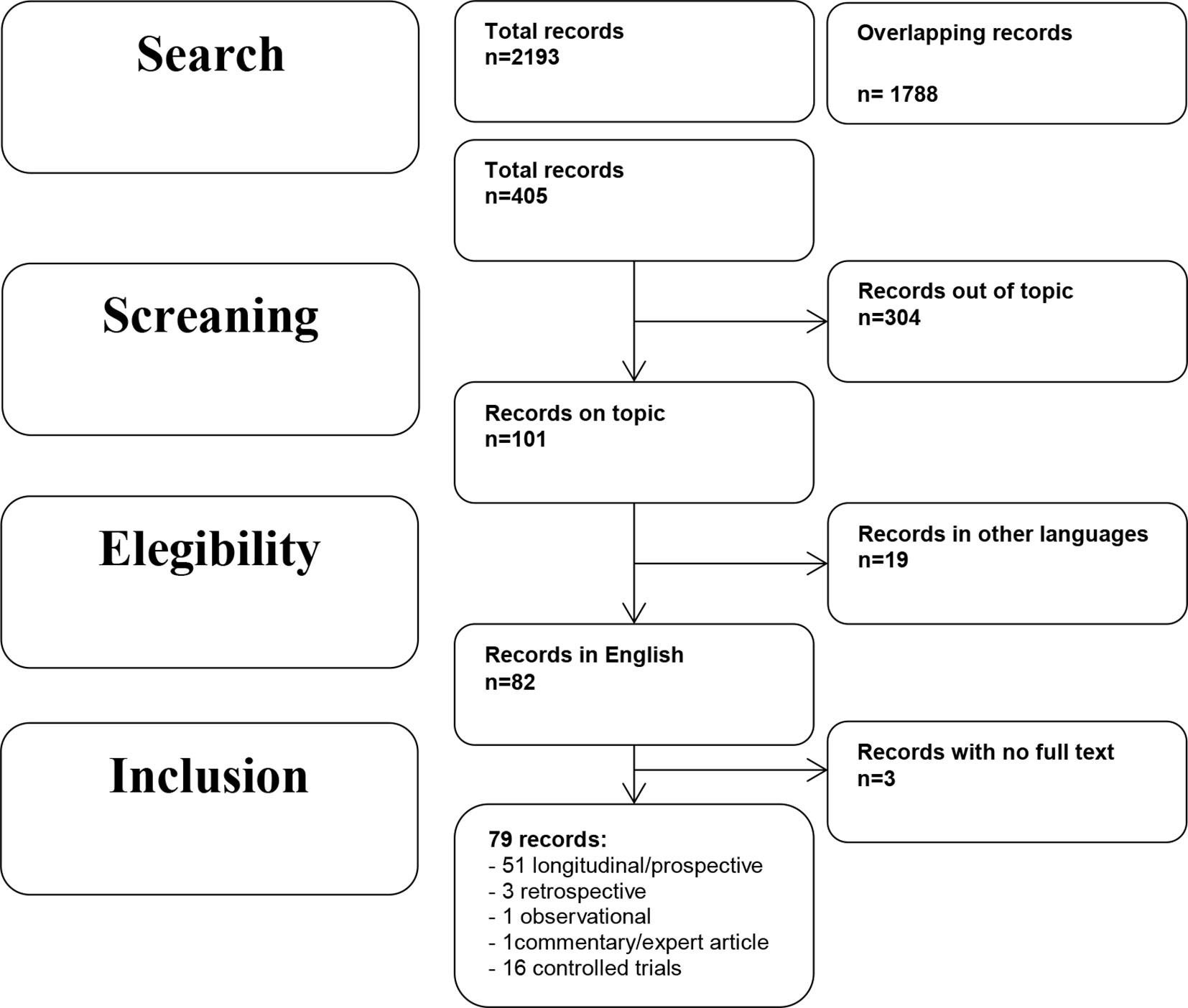
Figure 1 Literature search flowchart.
Precocious Environmental Factors
Several studies have identified a broad range of environmental factors that are related to subsequent risk for BPD, including socio-economic status, family psychopathology, parent-child relationship, and maltreatments or other traumatic events. In recent years, a growing number of investigations has been focused on the powerful role of social influences, particularly bullying and rejection by peer groups.
Family-Related Factors and Early BPD
Only two longitudinal studies specifically investigated the association between socioeconomic status (low income, low educational level, and low status occupation) and early onset of BPD. In the study performed by Cohen and collaborators ( 16 ) the authors examined the effects of familial socioeconomic status on the severity of schizotypal and borderline personality disorders symptoms in a general population of 608 children and adolescents living in urban, suburban, and rural residence. These subjects were longitudinally studied between ages 10 and 36. The authors concluded that lower socioeconomic status predicted BPD symptoms and the effect of magnitude remained stable over time. The same results were found in the second study with a similar design and objective in a large community sample of 766 children ( 17 ).
Other investigations evaluated the impact of family environment including economic adversities and parents’ psychopathology on precocious onset of BPD. Four studies were aimed to verify the association with poverty and maladaptive behaviours, such as hitting, shouting, hostility, and parent conflicts, on early BPD. One study was conducted in a large sample of 6,050 mothers and their children recruited in the community ( 18 ), while three investigations were performed in samples (ranged between 113 to 2,282 participants) of high-risk subjects ( 19 – 21 ). Winsper and colleagues ( 18 ) observed mothers and children for 12 years and found that family adversities and maladaptive parental behaviours predicted increased risk for BPD in very young age (11 years). Stepp and colleagues ( 19 – 21 ) showed that poverty condition that required public assistance may predict BPD symptoms during adolescence.
Theories on the role of parents’ psychopathology, in particular maternal BPD, as putative precursor to BPD in children and adolescents ( 22 , 23 ), have found empirical support from three longitudinal studies ( 24 – 26 ) and one controlled study ( 27 ). Barnow and colleagues ( 24 ) and Reinelt and collaborators ( 26 ) studied a large community sample (respectively, 286 and 295 subjects) during 5 years, while Stepp and colleagues’ study ( 25 ) included a sample of 816 subjects from the community who were observed for 16 years. Results were consistent in identifying maternal BPD as predictor of BPD onset in adolescence (15 years) ( 24 , 26 ) and early adulthood (24 years) ( 25 ). Mahan and colleagues ( 27 ) evaluated the association between maternal BPD, maternal psychological control, and onset of BPD in adolescence. The authors sampled 28 mothers with a diagnosis of BPD, 28 control comparisons, and their adolescent offspring. All subjects were assessed for borderline features. Maternal psychological control was found positively associated with borderline features of mothers and with affective instability of offspring with an increased risk for adolescents of developing BPD themselves.
The impact of other maternal psychopathological dimensions on BPD onset in adolescents was evaluated. In a study conducted in a high-risk sample of 700 youths that were studied from mid-adolescence to young adulthood, authors observed that maternal externalizing disorder and offspring internalizing disorder were significant associated with BPD risk ( 28 ). Study performed by Winsper and colleagues ( 9 ) showed that maternal anxiety and depression during pregnancy predict early BPD in sons/daughters. In a similar way, depressive symptoms and antisocial personality disorder (ASPD) in caregivers predicted the onset of BPD in adolescence (14–17 years) in a sample of 2,212 high-risk subjects ( 20 ). Actually, this relation was significant in bivariate analyses, but not in final analyses of Stepp’s study.
Other three longitudinal studies aimed to evaluate the effects of maternal ego integration and impulsivity, medical problems, and interpersonal disturbances in producing early BPD symptoms in children/adolescents did not find any significant association ( 17 , 29 , 30 ).
As regards relationship between parents and children, studies obtained controversial findings. Among seven investigations, four reported a significant association between dysfunctional parent-child relationship and development of precocious BPD symptoms. Stepp and colleagues ( 25 ) evaluated in a 16-year follow-up study whether cohesion, discord, and support in relationships had an impact on BPD onset in 816 subjects from the community. The authors found that mother-child discord predicted BPD at 30 years. In accordance with the environment-genes interactions theory, Hammen and collaborators ( 31 ) observed a significant association between low relationship quality and BPD onset at 20 years in 385 subjects who had a particular genotype for the oxytocin receptor gene (AA/AG). Higher level of role confusion and disoriented behaviours in parent-young adult interaction seems to predict early borderline symptoms, in particular self-injuries and suicidality in late adolescence ( 32 ). Moreover, in a naturalistic study on the effects of inadequate parent-child boundaries, relationships centered on guilt induction, psychological control, and triangulation (children who mediated parental marital conflict) were found associated with children’s BPD features in 301 adolescents with severe behavioural and emotional disorders ( 33 ). Divergent findings were reported by two studies that did not show any significant association between parent-child relationship and onset of BPD in young age ( 30 , 34 ).
Trauma-Related Factors and Early BPD
The role of early traumatic events and maltreatments in the onset, course, and pathogenesis of BPD was extensively examined by several studies. The World Health Organization categorized maltreatment into physical neglect, emotional neglect, emotional abuse, physical abuse, and sexual abuse ( 35 ). Children who are abused and/or neglected show deficits of functioning in several mental areas that are associated with BPD symptoms ( 36 – 40 ). Among 15 investigations on this topic, 5 did not report a significant correlation between maltreatment/trauma and BPD symptoms in childhood and adolescence. On the contrary, in 10 longitudinal studies with a duration ranged between 8 and 30 years in large community samples of children and adolescents (ranging between 113 and 2,764 participants) a significant relation was reported between early BPD onset and emotional and physical neglect and verbal abuse ( 30 , 41 – 43 ); cumulative traumas ( 15 ); emotional abuse ( 44 ); physical abuse ( 15 , 30 , 45 ); sexual abuse ( 15 , 20 , 30 , 44 ). Lyons-Ruth et al. ( 46 ) also stated that “abuse experiences could not account for the independent effect of early maternal withdrawal on borderline symptoms.” It is required that both abuse and these features of early caregiver–child interaction are present and produce their effects. Experiences of child abuse and neglect reciprocally interact with genes expressions influencing the emergence and timing of normal developmental processes and predicting child or adolescent borderline personality ( 47 ). Cicchetti and colleagues evaluated expression of the oxytocin receptor (OXTR) and the FK506 binding protein 5 (FKBP5) gene polymorphisms among 1,051 maltreated and non-maltreated children. Findings underlined the importance of the interaction between the genetic variants associated and maltreatment experiences in increasing the risk for early borderline symptomatology. Moreover, these associations were different between females and males ( 48 ). Females were more at risk for borderline symptoms when they add minor alleles of the two candidate genes. In contrast, males presented an increased for borderline symptoms when they presented major alleles. It is noticeable that the maltreatment-gene-gender interaction for females is consistent with a diathesis-stress model. In contrast, a different picture can be identified in males: frequent crossover interactions suggested a differential sensitivity to environment model.
In more recent years, particular attention was paid to the role of social group interactions, in particular peer relationships, in the development of psychiatric symptoms in childhood and adolescence. Dysfunctional relationships with peer may contribute to or promote the onset of BPD ( 2 , 49 ). Being bullied during childhood predicted high risk to develop BPD not only in adulthood ( 2 ) but also in early adolescence ( 50 – 54 ). Five longitudinal studies specifically investigated this topic. Wolke and collaborators ( 50 ) participated in a 12-year prospective study that recruited 6,050 mothers and offspring enrolled in the Avon Longitudinal of Parents and Children (ALSPAC) study. Findings showed that chronic exposure to peer victimization during childhood can be considered a risk factor for the development of BPD symptoms in childhood (12 years). Among the same subjects of ALSPAC, Lereya and collaborators ( 51 ) evaluated the effect of exposure to bully between 7 and 10 years of age in 4,810 children and adolescents. Authors concluded that being bullied during childhood increased the risk of self-injuries in late adolescence, particularly if there is a concomitant exposure to an adverse family environment. ALSPAC data was also used by Winsper and colleagues ( 52 ) to assess the relationships between childhood disregulated behaviours, environmental factors (including bully victimization), and presence of BPD symptoms at 11 years. Bully victimization significantly predicted BPD, depressive and psychotic symptoms in children who had disregulated behaviours. Similar findings were obtained by data from 875 participants to the McMaster Teen Study ( 53 ), in which the association between early BPD development and chronic bullying involvement was confirmed in children with a reactive temperament. Antila et al. ( 54 ) verified the association of bullying behaviour in adolescence and PDs in early adulthood with particular attention to gender differences in 508 inpatient adolescents. They concluded that female, but not male, victims of bullying had a fourfold increased risk to develop PD, including BPD, in young age.
In summary, among precocious environmental factors, the most strong associations with the early onset of BPD are represented by verbal, physical, sexual abuses, maternal withdrawal/neglect in childhood, and chronic exposure to peer bully victimization during infancy. In addition, a smaller number of studies in a wide sample of patients monitored for many years showed that maternal psychopathology (BPD and depression), economic adversities, and maladaptive parental behaviours promoted the early development of BPD in the offspring. It remains open and understudied how genetic factors may interact with the environmental factors in promoting precocious BPD symptoms. Results are displayed in Table 1 .
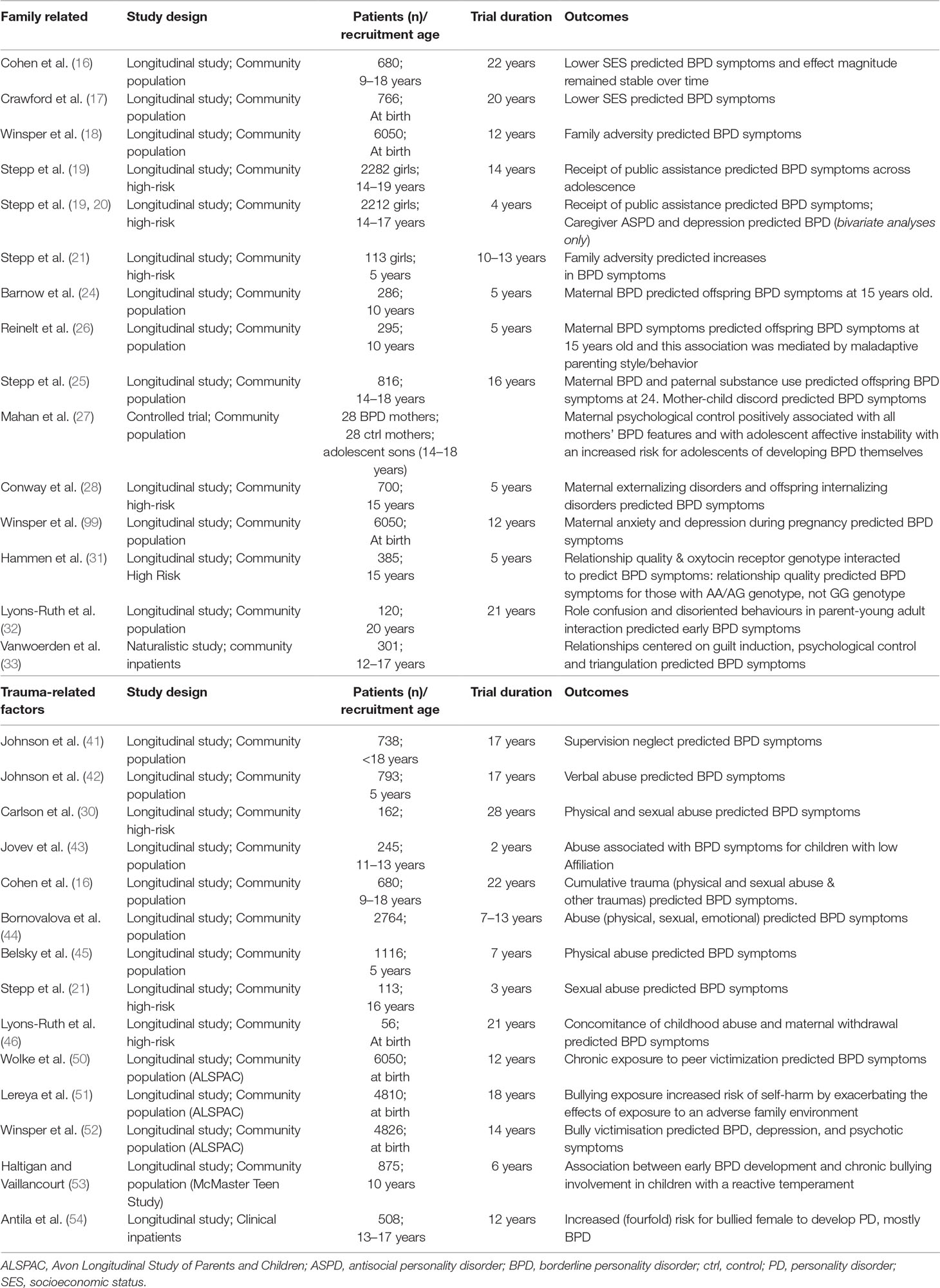
Table 1 Summary of studies on precocious environmental factors.
Child and Adolescent Temperament and Personality Factors
The investigation of intrapsychic factors, including temperamental characteristics and personality trait profiles in childhood and adolescence, is fundamental to recognize predictors of BPD at an early phase. Researchers identified several personality traits in children or adolescents, including affective instability, negative affectivity, negative emotionality, inappropriate anger, poor emotional control, impulsivity, and aggression, that could prepare to borderline pathology [e.g., Refs. ( 45 , 55 – 57 )]. Few studies evaluated the relation of childhood personality traits to BPD in adulthood ( 30 , 44 , 58 ). Fifteen investigations examined the relationship between temperament or personality features associated with early BPD symptoms. Only one study ( 30 ) did not find any significant association in the final analyses.
Two studies adopted the Cloninger’s model to evaluate the association between temperamental patterns in childhood or adolescence and onset of BPD ( 59 , 60 ). In the first study ( 59 ) temperamental characteristics were retrospectively collected in 180 depressed adult patients with personality disorders. Although it is hard to distinguish temperamental dimensions in personality of adult patients, authors found that high harm avoidance and novelty seeking (in combination with childhood experiences and adolescent psychopathology) can be considered predictive of early BPD. In line with this investigation, Kaess et al. ( 60 ) observed in a controlled study comparing 33 BPD adolescents, 35 clinical controls, and 31 healthy subjects that high harm avoidance and novelty seeking but low reward dependence represent a biological vulnerability for developing BPD.
Across other temperamental traits, aggressive behaviors in childhood and early adolescence was associated to onset of BPD. Crick and collaborators ( 55 ) investigated different subtypes of aggression in a prospective study that recruited 400 children and found that relational aggression, but not physical aggression, emerged as a significant predictor for BPD features. This result was confirmed by Underwood ( 61 ) in a prospective study with the same objective. Similarly, Cramer et al. ( 62 ) performed a longitudinal study, in which childhood personality traits were assessed at age 11 in 100 subjects and provided evidence that aggression and impulsivity are two predictive traits for BPD traits at 23 years. Vaillancourt and colleagues ( 57 ) prospectively found in 484 children and adolescents that aggression predicted the diagnosis of BPD at 14 years with some gender differences: relational aggression was the predominant predictor in boys, while physical aggression was the strongest predictor in girls.
Negative emotionality, in terms of negative affectivity and poor emotional control, is another important precocious factor associated to BPD onset. Lenzenweger and collaborators ( 22 ) conducted a community 3-year study with 250 adolescents/young adults, aimed to evaluate whether negative emotionality and other dimensions such as affiliation, constraint, and agency might impact on early onset of BPD. Findings showed that negative emotionality and low constraint predicted BPD at 19 years, and lower agency predicted increasing of BPD during time. Tragesser and collaborators ( 63 ) in a high-risk population of 353 subjects of 18 years reported a significant association of negative affectivity and impulsivity in childhood with BPD at 20 years. Similar findings were obtained by Stepp and collaborators in two following investigations ( 19 , 20 ) with a larger sample ranged between 2,212 and 2,282 children/adolescents. They confirmed the role of negative affectivity and impulsivity in predicting BPD, even at 14 years ( 19 ), and highlighted the importance of higher activity and lower sociability in childhood as precursors of the disorder. As concerns negative emotionality, the result was replicated in two following studies ( 5 , 64 ) with similar design and number of participants. In addition, Hallquist and colleagues ( 64 ) found that low self-control may predict BPD at 14 years and a worsening self-control increased BPD symptoms during the time.
Low self-control, impulsivity, and affective instability are three tightly connected dimensions that in very young age can be considered predictors for developing borderline pathology. Several investigations have assessed the influence of these constructs in childhood on later BPD symptoms. Tragesser and colleagues ( 65 ) reported that affective instability and impulsivity predicted BPD onset at 20 years. Gratz et al. ( 66 ) highlighted, in a sample of 263 children (9–13 years), the importance of interrelationship among these two relevant personality traits (affective instability and impulsivity) with low self- and emotion regulation, and with childhood borderline personality symptoms. Lower self-control and higher level of impulsivity were also identified as predictors of a diagnosis of BPD at 12 years in a 7 years twins study conducted in 1,116 children (around 5 years old) ( 45 ).
Only one study investigated the impact of anger, as temperamental trait, in childhood on BPD in adolescence/adulthood. Crawford and colleagues ( 17 ) showed a significant association between anger/tantrum dimension and BPD symptoms in 766 children who were followed for 20 years.
Five studies explored the interaction between child/adolescent personality traits and environmental or neurobiological factors in development of precocious BPD. Four investigations examined the effect of the relationships between temperamental characteristics and childhood maltreatment on the onset of BPD. Jovev et al. ( 43 ) studied the interaction between emotional control and affiliation traits, parental maltreatment and BPD in 245 children aged between 11 and 13 years. They observed that specific early temperamental features, particularly low emotional control, interact with familial maltreatment in promoting BPD symptoms across early to middle adolescence. On the other hand, parental abuse could have a moderating role in the presence of low affiliation. Martin-Blanco and colleagues ( 67 ) found in 130 subjects with early BPD that neuroticism-anxiety, aggression-hostility dimensions, and emotional abuse were independent risk factors associated with BPD. Two studies of the same year performed by Sharp et al. ( 68 ) and Stepp et al. ( 21 ) with different sample amplitude and duration, respectively, followed 730 adolescents for 1 year and 113 adolescents studied for 13 years and reported that the effect of lower self-control in promoting early onset of BPD was mediated by harsh familial discipline ( 68 ), and the impact of negative affectivity on early BPD was moderated by family adversities ( 21 ).
One study evaluated in 153 healthy adolescents the interaction of a temperamental risk factor and a neurobiological risk factor in predicting the emergence of BPD during early adolescence ( 69 ). Authors examined several temperamental factors and volumetric measures of hippocampal asymmetry. Results showed that subjects were more likely to have BPD symptoms in presence of high affiliation, low effortful control, and rightward hippocampal asymmetry.
In summary, temperamental traits in childhood, including relational aggression, impulsivity, low emotional control, and negative affectivity, are robust predictors of early onset of BPD. Some evidences support the role of the interaction between temperamental features (low emotional control, negative affectivity, and low affiliation) and familial environment (parental maltreatment, harsh discipline, and familial adversities) in developing BPD.
Early Psychopathological Features and Diagnosis
Available evidences highlighted that internalizing and externalizing psychopathology is often present before the onset of BPD in adolescents. Externalizing pathology includes conduct disturbances, oppositional defiant disorder, attention-deficit/hyperactivity symptoms, impulsive-aggressive behaviours, self-injuries, and substance use disorder; while internalizing pathology mainly involves depression and anxiety, but also dissociation and suicidality. In addition, obsessive–compulsive disorder, separation anxiety disorder, and social phobia were frequently observed in adolescent populations ( 2 , 11 , 70 , 71 ). Some authors suggested that internalizing and externalizing disorders emerge in pre-adolescence as anxiety and depressive symptoms in females, and ADHD, conduct problems in males. These disorders may form a platform on which develops personality pathology during adolescence ( 72 , 73 ). In the context of predisposing biological vulnerabilities and interacting stressful life events, these antecedent disorders represent a predisposing condition that, if untreated, may contribute to the onset of personality pathology during adolescence ( 73 ).
Seventeen investigations explored the psychopathological conditions predicting BPD in youths. Three of them did not find any significant association. One study investigated the effect of interaction of negative emotionality and internalizing psychopathology on early onset of BPD ( 25 ). Conway and collaborators ( 28 ) combined risk factors into a more comprehensive developmental model of borderline pathology in a community sample of 815 youths (15 years of age) at high risk for psychopathology due to maternal depression. In fact, they examined the effects between several environmental stressors, including occurrence of acute stressors and chronic stressors across individual, family, peer, and academic contexts, and personal characteristics to give a contribution to the hypothesis that BPD results from the complex interaction between pathogenic environments and individual vulnerabilities. Results showed that only adolescent internalizing psychopathology and trait of negative affectivity continued to predict borderline pathology after controlling for the presence of other risk factors. Krabbendam and colleagues ( 74 ) identified dissociation (internalizing symptom) significantly associated with onset of BPD at 20 years in a prospective study in which 184 adolescents were followed for 6 years. Self-injuries, another symptom related to internalizing psychopathology, was found predictive of early BPD in one investigation performed in 77 adolescent psychiatric inpatients and 50 young detainees ( 75 ). Sharp and colleagues ( 68 ) in a 1-year study including 730 adolescents (16 years) found that anxiety and depression (internalizing symptoms) predicted BPD at 17 years. Depression recurred as predictor of early BPD in other three studies ( 25 , 76 , 77 ) in samples including respectively 158, 524, and 816 subjects aged between 14 and 17 years. Studies lasted from 8 to 16 years of follow-up. In these investigations were identified as predictors of early BPD substance use disorder ( 25 , 76 , 78 ) and attention deficit hyperactivity disorder (ADHD) ( 77 ). It is noticeable that both internalizing and externalizing disorders are implicated in promoting BPD in young patients. Belsky and collaborators ( 45 ), Bornovalova and colleagues ( 78 ), and Bo and Kongerslev ( 79 ) confirmed the role of both internalizing and externalizing psychopathological conditions to predict early BPD. In particular, Bo and Kongerslev ( 79 ) compared 46 children and adolescents with BPD and 62 children and adolescents with other clinical conditions. Findings showed that high level of psychopathology (internalizing and externalizing), poor mentalizing abilities, and attachment problems were strictly associated to BPD in adolescents compared with psychiatric disorders other than BPD. In addition, Bornalova et al. ( 78 ) reported that higher number of BPD traits predicted earlier onset and faster worsening of substance use symptoms and that substance use slows the reduction of BPD traits in youths.
Some studies showed a significant association between externalizing pathologies and early onset of BPD. Miller and colleagues ( 80 ) observed a significant relationship between ADHD in childhood and BPD at 18 years in a 10 years follow-up study including 181 children. Two following studies ( 71 , 81 ) confirmed this association and also identified the oppositional defiant disorder in childhood as predictor of BPD respectively at 24 and 14 years. Similar findings were observed by Stepp and colleagues ( 20 ) that found a significant relationship of adolescent opposite defiant disorder and conduct disorder with BPD onset at age ranged between 14 and 17 years.
In the study performed by Wolke et al. ( 50 ) and described in the previous section, it was found that any Axis I diagnosis predicted BPD at very young age of 12 years. A recent controlled study performed by Thompson et al. ( 82 ) evaluated the prevalence of psychotic-like symptoms in 171 subjects of 15–18 years with BPD features. The authors found that adolescents with full-threshold BPD presented more confusion, paranoid ideation, visual hallucinations, and odd thoughts than adolescents with sub-threshold BPD symptoms and adolescents with no BPD symptoms.
In summary, among early psychopathological factors, both internalizing and externalizing disorders in childhood and adolescence are involved in producing early BPD in adult. In particular, the most robust associations are represented by depression, substance use disorder, ADHD, and oppositional defiant disorder. As the precise role of each of these potential etiological factors in determining risk for BPD is still unclear and there is a degree of overlap between them, their interaction with environmental stress has to be carefully considered. An additional hypothesis to explain the overlap of internalizing and externalizing disorders is that BPD pathology expresses itself in early stages of the disorder mainly with externalizing behaviours, although features of internalizing disorders are also present. When BPD adolescents grow up behavioral manifestations of externalizing disorders diminish in favour of a stronger expression of internalizing pathology ( 83 ). Result are displayed in Table 2 .
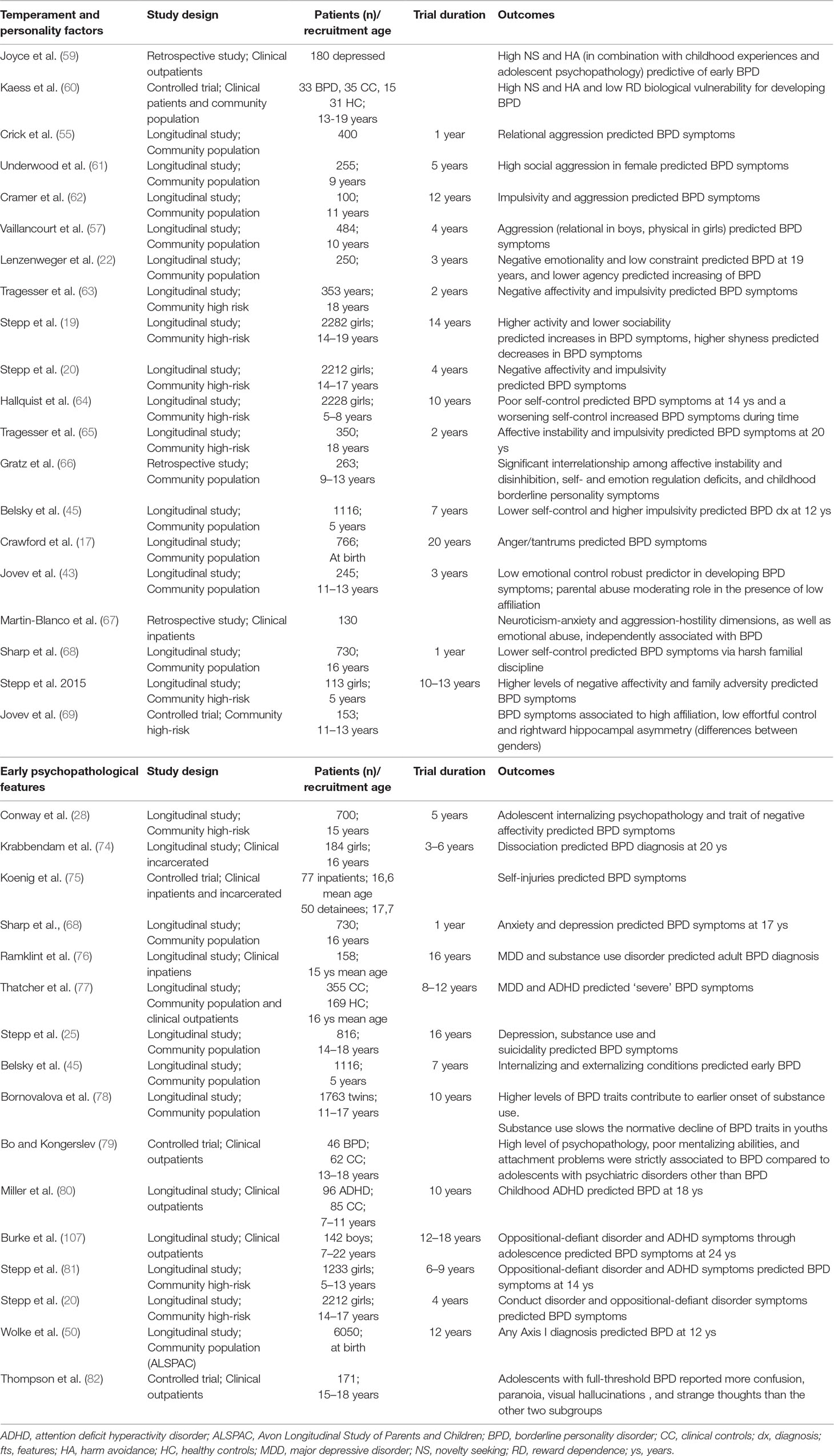
Table 2 Summary of studies on child and adolescent temperament and personality factors and early psychopathological features.
Neuroimaging and Early BPD
To date, no functional brain imaging studies have been published in adolescent populations with BPD. Neuroimaging studies of these subjects only focused on structural abnormalities, including both changes in grey and white matter.
It is interesting to evaluate the neurobiological underpinnings of younger populations with BPD symptoms at their beginnings in order to minimize the burden of confounders: some factors, such as prolonged duration of illness, pharmacotherapy, and recurring traumas, could themselves produce changes of brain structures ( 84 , 85 ).
Orbitofrontal cortex (OFC) was found reduced in volume by two studies which compared BPD to control groups ( 84 , 86 ). By means of region of interest (ROI) methodology, Chanen et al. ( 84 ) found that 20 BPD patients of 15–19 years showed a right-sided loss of OFC grey matter, reversing the normal (right > left) asymmetry of brain area volume, in comparison to 20 control subjects. In the study performed by Brunner et al. ( 86 ) using voxel-based morphometry (VBM) techniques, 20 BPD patients of 14–18 years displayed a significant shrinking of the left OFC and bilateral dorsolateral prefrontal cortex (DLPFC) compared with a group of 20 healthy controls. Authors found no differences between BPD group and 20 patients with other mental disorders. Using the same cohort of patients but varying imaging technics (diffusion tensor imaging, DTI), Maier-Hein et al. ( 87 ) found that the bilateral fornices of BPD group had lower myelination and their white matter bundles were less organized when compared to clinical and healthy controls. Thalamus and hippocampus, as well as the heteromodal association cortex, showed white matter disrupted connections in BPD patients. Such findings led the authors to argue that adolescents with BPD lack a normally functioning network involved in emotion processing. Reanalyzing the same data by means of another software, Richter et al. ( 85 ) found that BPD patients’ right amygdala was smaller than healthy (but not clinical) controls’ right amygdala. In the same study the authors demonstrated that hippocampal volume of BPD patients was the smaller in comparison to both control groups. In the same sample, Walterfang et al. ( 88 ) showed that BPD patients had the same dimension of corpus callosum as healthy controls.
Two studies reported a volume reduction of anterior cingulate cortex (ACC) ( 89 , 90 ) in adolescents with BPD. In the study performed by Whittle et al. ( 89 ) a shrinking in left AC cortex volume (across limbic and paralimbic regions) was found in 15 female patients (mean age 17,39) with BPD compared to 15 controls (mean age 19,65). Goodman et al. ( 90 ) found that 13 BPD/major depressive disorder (MDD) patients (mean age 15,8) had smaller relative volume in a part of the ACC, Brodmann area 24, in comparison to healthy subjects (mean age 16,2).
A study performed by Jovev et al. ( 43 ) has already been cited in a previous paragraph (see child and adolescent temperament and personality factors). The most important finding of the study is the moderator role of atypical rightward hippocampal asymmetry in the relationship between temperament traits and BPD symptoms in adolescents aged between 11 and 13 years. High scores in both affiliation and atypical rightward hippocampal asymmetry were good predictors of BPD symptoms in boys. For girls, low effortful control was linked to strong BPD symptoms in the presence of atypical rightward hippocampal asymmetry. It is noticeable that abnormalities of hippocampus are involved in memory processes and in emotional response to memories (emotional regulation and emotional recognition).
In a Diffusion Tensor Imaging (DTI) study, New et al. ( 91 ) observed bilateral tract specific decreased fractional anisotropy (FA) in the inferior longitudinal fasciculus (fibre bundle connecting the temporal lobe and occipital lobe) in 14 BPD adolescents in comparison to 13 controls. Moreover, a lower FA in the uncinate and occipitofrontal fasciculi (the white matter tracts connecting parts of the limbic system to the OFC among other frontal regions) was found at follow-up analysis in BPD adolescents.
Mainly in accordance with adult findings, studies discussed above showed structural anomalies both in grey and white matter of frontolimbic areas that are deeply involved in emotion regulation and impulse control. Even if no functional studies on BPD adolescents have been carried out yet, white matter alterations are compatible with functional findings in adults ( 92 ) displaying disruption in frontolimbic system connectivity. Result are displayed in Table 3 .
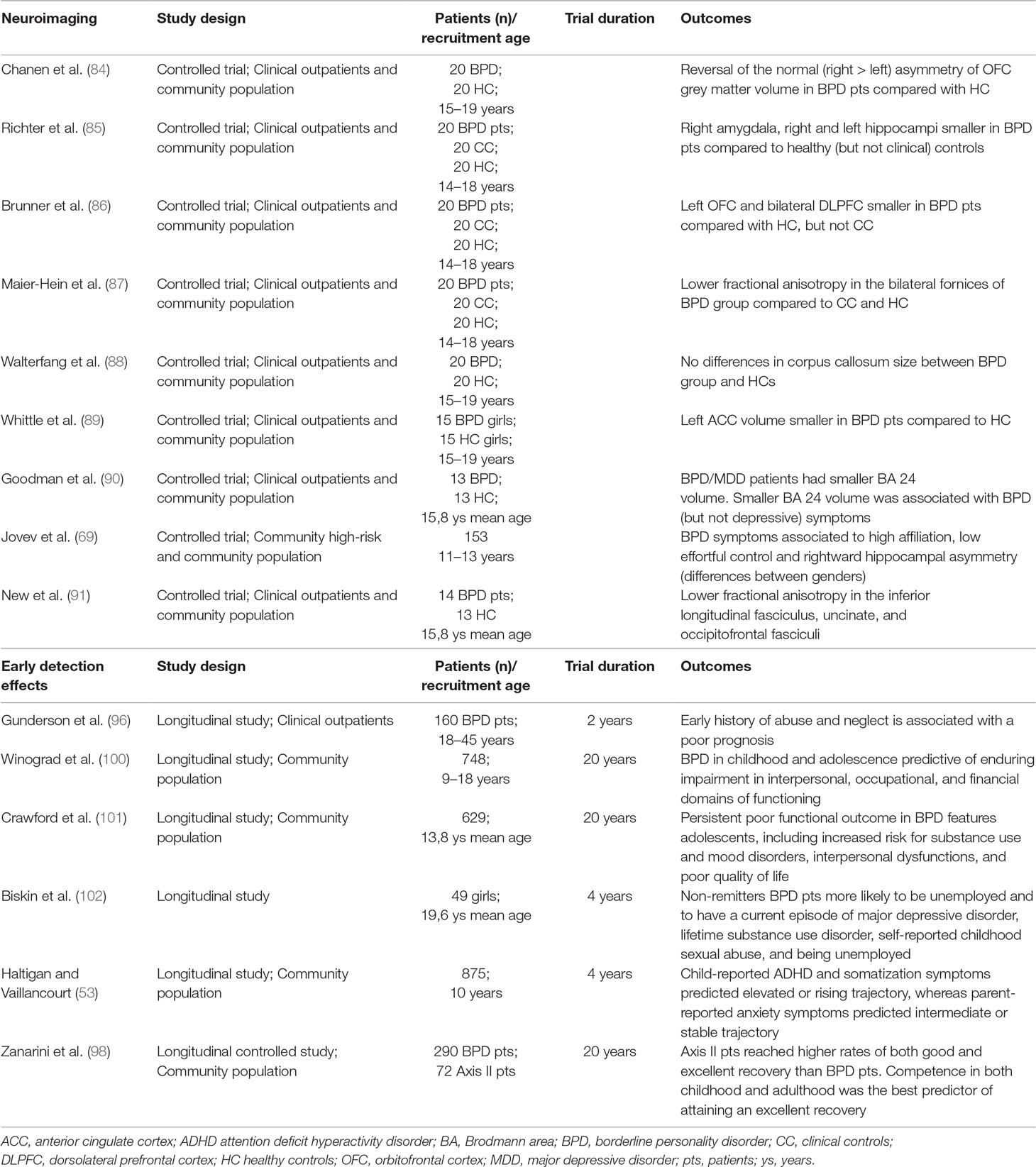
Table 3 Summary of studies on neuroimaging and effect of early detection on course and outcome of BPD.
Effect of Early Detection on Course and Outcome of BPD
Detecting personality abnormalities in childhood and adolescence is a challenge for clinicians and is crucial to increase our knowledge of personality psychopathology in adulthood. Several investigations suggested that generally BPD symptoms have their onset in adolescence, reach a peak in early adulthood, and then decline during the course of life ( 83 , 93 ). The decrease of BPD symptoms might be attributed to declining levels of impulsivity and dyscontrolled behaviors, while the persistence of a subsyndromal BPD is probably due to enduring negative affects ( 94 ). Other studies indicated that 20% of youths had an increase of PD symptoms over the decade from mid-adolescence to early adulthood ( 95 ). Only a few studies specifically investigated the effect of early onset on outcome and whether early factors may influence the trajectories of later BPD. In a 2-years follow-up study Gunderson et al. ( 96 ) found that an early history of abuse and neglect is associated with a poor prognosis in 160 adults with BPD. Among factors related to a poor long-term outcome, younger age at first treatment plays an important role together with affective instability, length of prior hospitalization, antisocial behaviors, comorbid substance use disorder, history of family psychiatric diseases, and dysfunctional relationship with parents ( 97 , 98 ). Available studies indicated that long-term (until 20 years) functioning does not reach a satisfactory level, even when BPD achieve the clinical remission ( 99 ). In particular, BPD in childhood and adolescence predicted a long-lasting impairment in relational, occupational, and economic domains, as resulted by investigation performed by Winograd and collaborators ( 100 ) in 748 subjects prospectively followed for 20 years. These findings are consistent with those obtained in the investigation published by Crawford and colleagues ( 101 ). The authors highlighted that poor functional outcome persists for many years in adolescents who presented borderline features, including risk for substance use, depressive symptoms, interpersonal dysfunctions, and poor quality of life. Furthermore, Biskin and colleagues ( 102 ) in a 4-years prospective study found that woman who received a diagnosis of BPD in adolescence (49 patients) were less likely to have a stable occupation in comparison with other psychiatric disorders. Haltigan and Vaillancourt ( 53 ) evaluated the associations of childhood risk factors and trajectories during 4 years of later BPD features in a 875 community-based sample. Authors identified three distinct trajectories on the basis of symptoms and severity of course of BPD: low or stable, intermediate or stable, and elevated or rising. Attention-deficit hyperactivity disorder (ADHD) and somatization symptoms reported by child predicted elevated or rising trajectory, whereas anxiety reported by parent and ADHD symptoms reported by child predicted intermediate or stable trajectory. Presence of somatization symptoms reported by child was the only factor to differentiate the intermediate or stable and elevated or rising trajectory groups and may predict histrionic traits and hypochondria in later BPD. Moreover, young subjects with a reactive temperament who experienced chronic bullying by peers were more likely to be in a rising/elevated BPD features trajectory group. In a recent long-term follow-up study, Zanarini and colleagues ( 98 ) examined two levels of positive outcome at 20 years: “good and excellent recovery” achieved by BPD patients in comparison with other personality disorders (controls). Results showed that controls reached superior rates of both “good and excellent recovery” than BPD patients and that high competence in both childhood and adulthood was the main predictor of excellent recovery. Predictors associated with competence were higher IQ, good childhood work competence, and temperamental features including neuroticism and agreeableness. In particular, pattern of lower neuroticism and higher agreeableness can be interpreted as protective temperamental factors in childhood that allow them to develop a stable and cohesive personality ( 98 , 103 , 104 ).
Conclusions
On the basis of the results discussed in the previous paragraphs, adolescence represents a sensitive and vulnerable phase for the development of BPD ( 83 ). In order to identify and monitor high-risk population from premorbid manifestations it is important to characterize and detect main associated risk factors for early BPD ( 99 , 105 ). Despite strong evidence supporting the benefits of early identification of BPD and the recommendations of treatment guidelines for BPD ( 10 , 106 ), fear of stigmatization still constitutes a barrier to early diagnosis in clinical practice ( 2 , 8 ). Different processes may contribute to the early onset of this personality disorder and several precocious risk factors are involved. Among family-related environmental factors, low socioeconomic status of family, economic adversities, and maladaptive behaviors in parents are three robust independent prospective risk factors for early BPD ( 16 – 21 ). Another significant precursor to BPD in childhood and adolescence is maternal psychopathology. The most significant result concerns the association between maternal BPD and offspring early BPD ( 24 – 26 ). The association between other maternal psychopathological conditions such as externalizing disorder history ( 28 ) and anxiety ( 9 ) with early BPD onset is still understudied. As concerns the relationships between parents and children, investigations obtained controversial results. Anyway, some kind of dysfunctional parent-child relationship was identified as a potential predictor of early BPD: discord between mother and child, significant role confusion, and disoriented behaviors in parents, inadequate parent-child boundaries, psychological control by parents, and low relationships quality in individuals with a particular genotype for the oxytocin receptor gene ( 25 , 31 – 34 ). Among trauma-related environmental factors, verbal abuse, emotional abuse, physical abuse, sexual abuse, and emotional and physical neglect were identified as potential risk factors for young BPD ( 16 , 21 , 30 , 41 , 42 , 44 , 45 , 48 ). Particular attention was paid to chronic exposure to peer victimization ( 49 – 54 , 60 ). Some authors highlighted the importance of gene-environment interaction in development of BPD. In fact, subjects with particular genotypes have a greater risk to develop BPD in presence of predisposing environment conditions ( 48 ).
With regard to child and adolescent-related factors, a number of studies identified as main predictors of BPD at an early stage the following temperamental traits: aggressiveness (in particular relational aggression) ( 55 , 57 , 61 , 62 ), impulsivity, affective instability, negative affectivity ( 5 , 19 , 22 , 45 , 63 – 65 ), and low emotional control by interaction with maltreatments ( 21 , 43 , 68 ).
Several psychopathological conditions in childhood and adolescence that potentially predict BPD were examined. Results showed that both internalizing (depression, anxiety, dissociation, self-harming) and externalizing (substance use disorder, ADHD, opposite defiant disorder, conduct disorder) disorders are involved in promoting BPD onset in young people ( 25 , 44 , 45 , 74 – 81 ).
Extensive overlap with internalizing and externalizing psychopathology in adolescence and early adulthood can produce noticeable difficulties in the diagnosis of BPD. The new alternative model of personality disorders proposed by DSM-5 could contribute to address these difficulties as it combines the traditional categorical approach with a dimensional traits model that is likely more sensitive to specific traits of early onset BPD. Of course this is only a hypothesis that needs to be confirmed by data.
Findings from neuroimaging studies allow us to verify that in adolescents with BPD are already present some abnormalities that we can find in adulthood. Available studies investigated only the structural aspects, as functional brain imaging studies have not been conducted in adolescents to our knowledge. The most important abnormalities concern fronto-limbic structures. In particular, the reduction of volume of OFC ( 84 , 86 ), ACC ( 89 , 90 ), and hippocampal asymmetry ( 43 ) were found in early BPD compared with controls. Also in white matter, some specific alterations were observed: inferior longitudinal fasciculus and the fornix showed a diminished fractional anisotropy in BPD adolescents compared with controls. These findings suggested that abnormalities in specific white matter pathways involved in emotion regulation could indicate that a wider network of emotion processing is dysfunctional in adolescents with BPD ( 2 ).
Evidence collected on the impact of early BPD onset on later functioning of patients are generally in accordance to retain that BPD in childhood and adolescence predict a severe impairment of interpersonal and occupational functioning ( 99 , 100 ), as well as younger age at first treatment, affective instability, antisocial behaviors, substance abuse, and dysfunctional relationships with parents ( 96 – 98 ). Furthermore, poor functional outcome persists up to 20 years into the future in individuals who presented BPD in adolescence ( 101 ). Some precocious protective factors related to childhood competence, such as higher IQ, good childhood work history, higher agreeableness, and lower neuroticism, were also identified ( 98 , 103 ).
In conclusion, specific BPD features emerge in childhood and adolescence. Recognizing these precocious predictors may have significant clinical implications. Early onset of this complex and serious personality disorder is associated with high risk of negative outcome and long-term poor psychosocial functioning. Precocious identification of BPD symptoms and accurate investigation of protective and risk factors is fundamental to promote prompt and adequate intervention programs and to improve the natural life-course trajectory of the disorder.
A Preliminary Model of Risk Factors in BPD
We tried to support the work of clinicians in this field by providing a synthetic summary of findings collected in the different clusters of risk factors. So, it should be easier to identify more common and significant associations in the clusters of environmental precocious factors, child and adolescent temperament and personality factors, early psychopathological features, and neuroimaging factors.
A further step that can be useful for clinicians to detect early clinical conditions and to implement preventive interventions consists in the proposal of a hypothetic model that represents a high-risk condition for the onset of BPD. This model is a combination of more important and common factors identified in literature and is supported by the idea that their interactive effects are stronger and more relevant than the separate effects of single factors. A reasonable hypothesis on the basis of available data is that high-risk subjects are characterized by a series of predisposing factors. The first factor to consider is a positive history of early traumatic experiences. According to the more common findings in literature, early trauma can be represented by conditions of abuse or neglect in childhood or adolescence, or can be the consequence of persistent abnormalities in familial behaviors and relationships due to severe mother psychopathology. The effects of traumatic experiences are substantially increased when they do not occur as isolated events, but when the dysfunctional familial environment that produces traumas interacts with the child’s innate temperamental features. In this case, authors have identified a significant role for three temperamental traits: impulsive aggression, inadequate emotional control, and negative affectivity. Another relevant factor that can combine its effects with the previously reported environmental and temperamental dysfunctions to enhance the risk of early onset BPD is the occurrence in childhood/adolescence of precocious internalizing and externalizing psychiatric disorders. Particular attention has been received by depression, ADHD, and substance use disorder, that all represent psychopathological conditions with a frequent onset in early age, but a long-lasting association with symptoms of BPD in adulthood. We can suggest that some of these disorders are not independent comorbidities, but must be conceptualized as precocious expressions of BPD pathology. A few studies indicated that studies of neuroimaging can contribute to identify which brain structures are altered in subjects with risk factors for early onset BPD. For example, structural abnormalities of fronto-limbic areas have been related to impulsive and emotional dysregulation. If these changes of brain structures are specific enough, they will contribute to identify biological markers or neural signatures, a primary goal in psychiatric and brain imaging research. Of course, it must be noticed that we present here only a hypothetical model with the main purpose to stimulate the interest of researchers and the debate among experts. The indicators of a high-risk condition for early onset of BPD, and particularly the effects of their coexistence and interaction in the proposed model, must be furtherly investigated and confirmed in specific studies. One of the more challenging issues at the present state of our knowledge is to make clear which of the factors proposed in this model have a primary role in the pathogenesis of BPD and which intervene only at a later time to augment and trigger the effects of primary factors.
An important contribution to understand the complex effects of temperamental traits, traumatic experiences, and environmental dysfunctions on the neurobiology of young BPD patients could derive from studies of functional changes in brain areas during administration of specific stimuli ( 108 ). For example, studies of autobiographical memories in such populations could be of great value to investigate the effects of life events and traumatic experiences on the function of fronto-limbic brain structures involved in the construction of identity.
Author Contributions
PB and SB equally contributed to summarizing the literature data and writing the review. MB collected literature data and organized the tables. PR contributed to writing and supervising the review.
This study was supported by Ministero dell’Istruzione, dell’Università e della Ricerca-MIUR projects “Dipartimenti di Eccellenza 2018-2022” to the Department of Neuroscience “Rita Levi Montalcini.”
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: Author (2013). doi: 10.1176/appi.books.9780890425596
CrossRef Full Text | Google Scholar
2. Kaess M, Brunner R, Chanen AM. Borderline personality disorder in adolescence. Pediatrics (2014) 134(4):782–93. doi: 10.1542/peds.2013-3677
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: diagnosing borderline personality disorder in adolescents. Clin Psychol Rev (2008) 28(6):969–81. doi: 10.1016/j.cpr.2008.02.004
4. Stepp SD, Lazarus SA, Byrd AL. A systematic review of risk factors prospectively associated with borderline personality disorder: taking stock and moving forward. Personal Disord (2016) 4:316–23. doi: 10.1037/per0000186
5. Stepp SD, Lazarus SA. Identifying a borderline personality disorder prodrome: implications for community screening. Personal Ment Health (2018) 11:195–205. doi: 10.1002/pmh.1389
6. Johnson JG, Cohen P, Kasen S, Skodol AE, Oldham JM. Cumulative prevalence of personality disorders between adolescence and adulthood. Acta Psychiatr Scand (2008) 118(5):410–3. doi: 10.1111/j.1600-0447.2008.01231.x
7. Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder in Great Britain. Br J Psychiatry (2006) 188:423–31. doi: 10.1192/bjp.188.5.423
8. Chanen AM, McCutcheon LK. Personality disorder in adolescence: the diagnosis that dare not speak its name. Pers Ment Health (2008) 2(1):35–41. doi: 10.1002/pmh.28
9. Winsper C, Wolke D, Lereya T. Prospective associations between prenatal adversities and borderline personality disorder at 11-12 years. Psychol Med (2015) 45(5):1025–37. doi: 10.1017/S0033291714002128
10. Zanarini MC, Temes CM, Frankenburg FR, Reich DB, Fitzmaurice GM. Description and prediction of time-to-attainment of excellent recovery for borderline patients followed prospectively for 20 years. Psychiatr Res (2018) 262:40–5. doi: 10.1016/j.psychres.2018.01.034
11. Fonagy P, Speranza M, Luyten P, Kaess M, Hessels C, Bohus M. Borderline personality disorder in adolescence: an expert research review with implications for clinical practice. Eur Child Adolesc Psychiatry (2015) 24:1307–20. doi: 10.1007/s00787-015-0751-z
12. Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Compr Psychiatry (2001) 42(2):144–50. doi: 10.1053/comp.2001.19749
13. Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. The Personality Disorders Institute/Borderline Personality Disorder Research Foundation randomized control trial for borderline personality disorder: rationale, methods, and patient characteristics. J Pers Disord (2004) 18(1):52–72. doi: 10.1521/pedi.18.1.52.32769
14. Sharp C, Mosko O, Chang B, Ha C. The cross-informant concordance and concurrent validity of the Borderline Personality Features Scale for Children in a community sample of boys. Clin Child Psychol Psychiatry (2011) 16(3):335–49. doi: 10.1177/1359104510366279
15. Chang B, Sharp C, Ha C. The criterion validity of the Borderline Personality Features Scale for Children in an adolescent inpatient setting. J Pers Disord (2011) 25(4):492–503. doi: 10.1521/pedi.2011.25.4.492
16. Cohen P, Chen H, Gordon K, Johnson J, Brook J, Kasen S. Socioeconomic background and the developmental course of schizotypal and borderline personality disorder symptoms. Dev Psychopathol (2008) 20(2):633–50. doi: 10.1017/S095457940800031X
17. Crawford T, Cohen P, Chen H, Anglin D, Ehrensaft M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Dev Psychopathol (2009) 21(3):1013–30. doi: 10.1017/S0954579409000546
18. Winsper C, Zanarini MC, Wolke D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a non-clinical population at 11 years. Psychol Med (2012) 42(11):2405–20. doi: 10.1017/S0033291712000542
19. Stepp SD, Keenan K, Hipwell AE. & Krueger RF. The impact of childhood temperament on the development of borderline personality disorder symptoms over the course of adolescence. Borderline Pers Disord Emot Dysregul (2014a) 1(1):18–0. doi: 10.1186/2051-6673-1-18
20. Stepp SD, Whalen DJ, Scott LN, Zalewski M, Loeber R, Hipwell AE. Reciprocal effects of parenting and borderline personality disorder symptoms in adolescent girls. Dev Psychopathol (2014b) 26(2):361–78. doi: 10.1017/S0954579413001041
21. Stepp SD, Scott LN, Jones NP, Whalen DJ, Hipwell AE. Negative emotional reactivity as a marker of vulnerability in the development of borderline personality disorder symptoms. Dev Psychopathol (2016) 28(1):213–24. doi: 10.1017/S0954579415000395
22. Lenzenweger MF, Cicchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Dev Psychopathol (2005) 7(4):893–8. doi: 10.1017/S095457940505042X
23. Macfie J. Development in children and adolescents whose mothers have borderline personality disorder. Child Dev Perspect (2009) 3(1):66. doi: 10.1111/j.1750-8606.2008.00079.x
24. Barnow S, Aldinger M, Arens EA, Ulrich I, Spitzer C, Grabe HJ, et al. Maternal transmission of borderline personality disorder symptoms in the community-based Greifswald Family Study. J Pers Disord (2013) 27(6):806–19. doi: 10.1521/pedi_2012_26_058
25. Stepp SD, Olino TM, Klein DN, Seeley JR, Lewinsohn PM. Unique influences of adolescent antecedents on adult borderline personality disorder features. Personal Disord (2013) 4(3):223–9. doi: 10.1037/per0000015
26. Reinelt E, Stopsack M, Aldinger M, Ulrich I, Grabe HJ, Barnow S. Longitudinal transmission pathways of borderline personality disorder symptoms: from mother to child? Psychopathology (2014) 47(1):10–6. doi: 10.1159/000345857
27. Mahan RM, Kors SB, Simmons ML, Macfie J. Maternal psychological control, maternal borderline personality disorder, and adolescent borderline features. Personal Disord (2018) 9(4):297–304. doi: 10.1037/per0000269
28. Conway CC, Hammen C, Brennan PA. Adolescent precursors of adult borderline personality pathology in a high-risk community sample. J Pers Disord (2015) 29(3):316–33. doi: 10.1521/pedi_2014_28_158
29. Bezirganian S, Cohen P, Brook JS. The impact of mother-child interaction on the development of borderline personality disorder. Am J Psychiatry (1993) 150(12):1836–42. doi: 10.1176/ajp.150.12.1836
30. Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Dev Psychopathol (2009) 21(4):1311–34. doi: 10.1017/S0954579409990174
31. Hammen C, Bower JE, Cole SW. Oxytocin receptor gene variation and differential susceptibility to family environment in predicting youth borderline symptoms. J Pers Disord (2015) 29(2):177–92. doi: 10.1521/pedi_2014_28_152
32. Lyons-Ruth K, Brumariu LE, Bureau JF, Hennighausen K, Holmes B. Role confusion and disorientation in young adult-parent interaction among individuals with borderline symptomatology. J Pers Disord (2015) 29(5):641–62. doi: 10.1521/pedi_2014_28_165
33. Vanwoerden S, Kalpakci A, Sharp C. The relations between inadequate parent-child boundaries and borderline personality disorder in adolescence. Psychiatr Res (2017) 257:462–71. doi: 10.1016/j.psychres.2017.08.015
34. Greenfield B, Henry M, Lis E, Slatkoff J, Guilé JM, Dougherty G, et al. Correlates, stability and predictors of borderline personality disorder among previously suicidal youth. Eur Child Adolesc Psychiatry (2015) 24(4):397–406. doi: 10.1007/s00787-014-0589-9
35. Leeb RT, Barker LE, Strine TW. The effect of childhood physical and sexual abuse on adolescent weapon carrying. J Adolesc Health (2007) 40(6):551–8. doi: 10.1016/j.jadohealth.2007.01.006
36. Bradley B, DeFife JA, Guarnaccia C, Phifer J, Fani N, Ressler KJ, et al. Emotion dysregulation and negative affect: association with psychiatric symptoms. J Clin Psychiatry (2011) 72(5):685–91. doi: 10.4088/JCP.10m06409blu
37. Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA (2001) 286(24):3089–96. doi: 10.1001/jama.286.24.3089
38. Evans E, Hawton K, Rodham K. Suicidal phenomena and abuse in adolescents: a review of epidemiological studies. Child Abuse Negl (2005) 29(1):45–58. doi: 10.1016/j.chiabu.2004.06.014
39. Johnson RM, Kotch JB, Catellier DJ, Winsor JR, Dufort V, Hunter W, et al. Adverse behavioral and emotional outcomes from child abuse and witnessed violence. Child Maltreat (2002) 7(3):179–86. doi: 10.1177/1077559502007003001
40. Rogosch FA, Cicchetti D. Child maltreatment and emergent personality organization: perspectives from the five-factor model. J Abnorm Child Psychol (2004) 32(2):123–45. doi: 10.1023/B:JACP.0000019766.47625.40
41. Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: findings of a community-based longitudinal study. J Pers Disord (2000) 14(2):171–87. doi: 10.1521/pedi.2000.14.2.171
42. Johnson JG, Cohen P, Smailes EM, Skodol AE, Brown J, Oldham JM. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Compr Psychiatry (2001) 42(1):16–23. doi: 10.1053/comp.2001.19755
43. Jovev M, McKenzie T, Whittle S, Simmons JG, Allen NB, Chanen AM. Temperament and maltreatment in the emergence of borderline and antisocial personality pathology during early adolescence. J Can Acad Child Adolesc Psychiatry (2013) 22(3):220–9.
PubMed Abstract | Google Scholar
44. Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono WJ. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: a longitudinal discordant twin design. Abnorm Psychol (2013) 122(1):180–94. doi: 10.1037/a0028328
45. Belsky DW, Caspi A, Arseneault L, Bleidorn W, Fonagy P, Goodman M, et al. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Dev Psychopathol (2012) 24(1):251–65. doi: 10.1017/S0954579411000812
46. Lyons-Ruth K, Bureau JF, Holmes B, Easterbrooks A, Brooks NH. Borderline symptoms and suicidality/self-injury in late adolescence: prospectively observed relationship correlates in infancy and childhood. Psychiatr Res (2013) 206(2-3):273–81. doi: 10.1016/j.psychres.2012.09.030
47. Valentino K, Cicchetti D, Toth SL, Rogosch FA. Mother-child play and emerging social behaviors among infants from maltreating families. Dev Psychol (2006) 42(3):474–85. doi: 10.1037/0012-1649.42.3.474
48. Cicchetti D, Rogosch FA, Hecht KF, Crick NR, Hetzel S. Moderation of maltreatment effects on childhood borderline personality symptoms by gender and oxytocin receptor and FK506 binding protein 5 genes. Dev Psychopathol (2014) 26(3):831–49. doi: 10.1017/S095457941400042X
49. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: elaborating and extending Linehan’s theory. Psychol Bull (2009) 135:495–510. doi: 10.1037/a0015616
50. Wolke D, Schreier A, Zanarini MC, Winsper C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: a prospective study. J Child Psychol Psychiatry (2012) 53(8):846–55. doi: 10.1111/j.1469-7610.2012.02542.x
51. Lereya ST, Winsper C, Heron J, Lewis G, Gunnell D, Fisher HL, et al. Being bullied during childhood and the prospective pathways to self-harm in late adolescence. J Am Acad Child Adolesc Psychiatry (2013) 52(6):608–18. doi: 10.1016/j.jaac.2013.03.012
52. Winsper C, Hall J, Strauss VY, Wolke D. Aetiological pathways to Borderline Personality Disorder symptoms in early adolescence: childhood dysregulated behaviour, maladaptive parenting and bully victimisation. Borderline Pers Disord Emot Dysregul (2017) 3;4:10. doi: 10.1186/s40479-017-0060-x
53. Haltigan JD, Vaillancourt T. Identifying trajectories of borderline personality features in adolescence: antecedent and interactive risk factors. Can J Psychiatry (2016) 61(3):166–75. doi: 10.1177/0706743715625953
54. Antila H, Arola R, Hakko H, Riala K, Riipinen P, Kantojärvi L. Bullying involvement in relation to personality disorders: a prospective follow-up of 508 inpatient adolescents. Eur Child Adolesc Psychiatry (2017) 26(7):779–89. doi: 10.1007/s00787-017-0946-6
55. Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: a short-term longitudinal study. Dev Psychopathol (2005) 17(4):1051–70. doi: 10.1017/S0954579405050492
56. Nelson DA, Coyne SM, Swanson SM, Hart CH, Olsen JA. Parenting, relational aggression, and borderline personality features: associations over time in a Russian longitudinal sample. Dev Psychopathol (2014) 26(3):773–87. doi: 10.1017/S0954579414000388
57. Vaillancourt T, Brittain HL, McDougall P, Krygsman A, Boylan K, Duku E, et al. Predicting borderline personality disorder symptoms in adolescents from childhood physical and relational aggression, depression, and attention-deficit/hyperactivity disorder. Dev Psychopathol (2014) 26(3):817–30. doi: 10.1017/S0954579414000418
58. Conway CC, Hipwell AE, Stepp SD. Seven-year course of borderline personality disorder features: borderline pathology is as unstable as depression during adolescence. Clin Psychol Sci (2017) 5(4):742–9. doi: 10.1177/2167702617691546
59. Joyce PR, McKenzie JM, Luty SE, Mulder RT, Carter JD, Sullivan PF, et al. Temperament, childhood environment and psychopathology as risk factors for avoidant and borderline personality disorders. Aust N Z J Psychiatry (2003) 37(6):756–64. doi: 10.1111/j.1440-1614.2003.01263.x
60. Kaess M, Resch F, Parzer P, von Ceumern-Lindenstjerna IA, Henze R, Brunner R. Temperamental patterns in female adolescents with borderline personality disorder. J Nerv Ment Dis (2013) 201(2):109–15. doi: 10.1097/NMD.0b013e31827f6480
61. Underwood MK, Beron KJ, Rosen LH. Joint trajectories for social and physical aggression as predictors of adolescent maladjustment: internalizing symptoms, rule-breaking behaviors, and borderline and narcissistic personality features. Dev Psychopathol (2011) 23(2):659–78. doi: 10.1017/S095457941100023X
62. Cramer P. Childhood precursors of adult borderline personality disorder features: a longitudinal study. J Nerv Ment Dis (2016) 204(7):494–9. doi: 10.1097/NMD.0000000000000514
63. Tragesser SL, Solhan M, Brown WC, Tomko RL, Bagge C, Trull TJ. Longitudinal associations in borderline personality disorder features: Diagnostic Interview for Borderlines-Revised (DIB-R) scores over time. J Pers Disord (2010) 24(3):377–91. doi: 10.1521/pedi.2010.24.3.377
64. Hallquist MN, Hipwell AE, Stepp SD. Poor self-control and harsh punishment in childhood prospectively predict borderline personality symptoms in adolescent girls. J Abnorm Psychol (2015) 124(3):549–64. doi: 10.1037/abn0000058
65. Tragesser SL, Solhan M, Schwartz-Mette R, Trull TJ. The role of affective instability and impulsivity in predicting future BPD features. J Pers Disord (2007) 21(6):603–14. doi: 10.1521/pedi.2007.21.6.603
66. Gratz KL, Tull MT, Reynolds EK, Bagge CL, Latzman RD, Daughters SB, et al. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: the roles of affective dysfunction, disinhibition, and self- and emotion-regulation deficits. Dev Psychopathol (2009) 21(4):1263–91. doi: 10.1017/S0954579409990150
67. Martín-Blanco A, Soler J, Villalta L, Feliu-Soler A, Elices M, Pérez V, et al. Exploring the interaction between childhood maltreatment and temperamental traits on the severity of borderline personality disorder. Compr Psychiatry (2014) 55(2):311–8. doi: 10.1016/j.comppsych.2013.08.026
68. Sharp C, Kalpakci A, Mellick W, Venta A, Temple JR. First evidence of a prospective relation between avoidance of internal states and borderline personality disorder features in adolescents. Eur Child Adolesc Psychiatry (2015) 24(3):283–90. doi: 10.1007/s00787-014-0574-3
69. Jovev M, Whittle S, Yücel M, Simmons JG, Allen NB, Chanen AM. The relationship between hippocampal asymmetry and temperament in adolescent borderline and antisocial personality pathology. Dev Psychopathol (2014) 26:275–85. doi: 10.1017/S0954579413000886
70. Chanen AM, Jovev M, Jackson HJ. Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. J Clin Psychiatry (2007) 68(2):297–306. doi: 10.4088/JCP.v68n0217
71. Ha C, Balderas JC, Zanarini MC, Oldham J, Sharp C. Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. J Clin Psychiatry (2014) 75(5):e457–64. doi: 10.4088/JCP.13m08696
72. Livesley WJ, Jang KL. Toward an empirically based classification of personality disorder. J Pers Disord (2000) 14(2):137–51. doi: 10.1521/pedi.2000.14.2.137
73. Sharp C, Wall K. Personality pathology grows up: adolescence as a sensitive period. Curr Opin Psychol (2018) 21:111–6. doi: 10.1016/j.copsyc.2017.11.010
74. Krabbendam AA, Colins OF, Doreleijers TA, van der Molen E, Beekman AT, Vermeiren RR. Personality disorders in previously detained adolescent females: a prospective study. Am J Orthopsychiatry (2015) 85(1):63–71. doi: 10.1037/ort0000032
75. Koenig J, Brunner R, Schmidt JM, Parzer P, Resch F, Kaess M. Psychopathology and borderline personality pathology associated with lifetime self-injurious behavior in adolescent psychiatric inpatients and detainees. Z Kinder Jugendpsychiatr Psychother (2017) 45(6):441–51. doi: 10.1024/1422-4917/a000549
76. Ramklint M, von Knorring AL, von Knorring L, Ekselius L. Child and adolescent psychiatric disorders predicting adult personality disorder: a follow-up study. Nord J Psychiatry (2003) 57(1):23–8. doi: 10.1080/psc.57.1.23
77. Thatcher DL, Cornelius JR, Clark DB. Adolescent alcohol use disorders predict adult borderline personality. Addict Behav (2005) 30(9):1709–24. doi: 10.1016/j.addbeh.2005.07.008
78. Bornovalova MA, Verhulst B, Webber T, McGue M, Iacono WG, Hicks BM. Genetic and environmental influences on the co-development between borderline personality disorder traits, major depression symptoms, and substance use disorder symptoms from adolescence to young adulthood. Dev Psychopathol (2018) 30(1):49–65. doi: 10.1017/S0954579417000463
79. Bo S, Kongerslev M. Self-reported patterns of impairments in mentalization, attachment, and psychopathology among clinically referred adolescents with and without borderline personality pathology. Borderline Pers Disord Emot Dysregul (2017) 14;4:4. doi: 10.1186/s40479-017-0055-7
80. Miller CJ, Flory JD, Miller SR, Harty SC, Newcorn JH, Halperin JM. Childhood attention-deficit/hyperactivity disorder and the emergence of personality disorders in adolescence: a prospective follow-up study. J Clin Psychiatry (2008) 69(9):1477–84. doi: 10.4088/JCP.v69n0916
81. Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. J Abnorm Child Psychol (2012) 40(1):7–20. doi: 10.1007/s10802-011-9530-6
82. Thompson KN, Cavelti M, Chanen AM. Psychotic symptoms in adolescents with borderline personality disorder features. Eur Child Adolesc Psychiatry (2018). 28(7):985–99. doi: 10.1007/s00787-018-1257-2
83. Sharp C, Fonagy P. Practitioner Review: Borderline personality disorder in adolescence–recent conceptualization, intervention, and implications for clinical practice. J Child Psychol Psychiatry (2015) 56(12):1266–88. doi: 10.1111/jcpp.12449
84. Chanen AM, Velakoulis D, Carison K, Gaunson K, Wood SJ, Yuen HP, et al. Orbitofrontal, amygdala and hippocampal volumes in teenagers with first-presentation borderline personality disorder. Psychiat Res Neuroimaging (2008) 163:116–25. doi: 10.1016/j.pscychresns.2007.08.007
85. Richter J, Brunner R, Parzer P, Resch F, Stieltjes B, Henze R. Reduced cortical and subcortical volumes in female adolescents with borderline personality disorder. Psychiat Res Neuroimaging (2014) 221:179–86. doi: 10.1016/j.pscychresns.2014.01.006
86. Brunner R, Henze R, Parzer P, Kramer J, Feigl N, Lutz K, et al. Reduced prefrontal and orbitofrontal gray matter in female adolescents with borderline personality disorder: is it disorder specific? Neuroimage (2010) 49:114–20. doi: 10.1016/j.neuroimage.2009.07.070
87. Maier-Hein KH, Brunner R, Lutz K, Henze R, Parzer P, Feigl N, et al. Disorder-specific white matter alterations in adolescent borderline personality disorder. Biol Psychiatry (2014) 75:81–8. doi: 10.1016/j.biopsych.2013.03.031
88. Walterfang M, Chanen AM, Barton S, Wood AG, Jones S, Reutens DC, et al. Corpus callosum morphology and relationship to orbitofrontal and lateral ventricular volume in teenagers with first-presentation borderline personality disorder. Psychiat Res Neuroimaging (2010) 183:30–7. doi: 10.1016/j.pscychresns.2010.04.001
89. Whittle S, Chanen AM, Fornito A, McGorry PD, Pantelis C, Yücel M. Anterior cingulate volume in adolescents with first-presentation borderline personality disorder. Psychiat Res Neuroimaging (2009) 172:155–60. doi: 10.1016/j.pscychresns.2008.12.004
90. Goodman M, Hazlett EA, Avedon JB, Siever DR, Chu KW, New AS. Anterior cingulate volume reduction in adolescents with borderline personality disorder and comorbid major depression. J Psychiat Res (2011) 45:803–7. doi: 10.1016/j.jpsychires.2010.11.011
91. New AS, Carpenter DM, Perez-Rodriguez MM, Ripoll LH, Avedon J, Patil U, et al. Developmental differences in diffusion tensor imaging parameters in borderline personality disorder. J Psychiat Res (2013) 47:1101–9. doi: 10.1016/j.jpsychires.2013.03.021
92. Silbersweig D, Clarkin JF, Goldstein M, Kernberg OF, Tuescher O, Levy KN, et al. Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. Am J Psychiatry (2007) 164(12):1832–41. doi: 10.1176/appi.ajp.2007.06010126
93. Chanen AM, Kaess M. Developmental pathways to borderline personality disorder. Curr Psychiatry Rep (2012) 14(1):45–53. doi: 10.1007/s11920-011-0242-y
94. Arens EA, Stopsack M, Spitzer C, Appel K, Dudeck M, Völzke H, et al. Borderline personality disorder in four different age groups: a cross-sectional study of community residents in Germany. J Pers Disord (2013) 27(2):196–207. doi: 10.1521/pedi_2013_27_072
95. Cohen P, Crawford TN, Johnson JG, Kasen S. The children in the community study of developmental course of personality disorder. J Pers Disord (2005) 19(5):466–86. doi: 10.1521/pedi.2005.19.5.466
96. Gunderson JG, Daversa MT, Grilo CM, McGlashan TH, Zanarini MC, Shea MT, et al. Predictors of 2-year outcome for patients with borderline personality disorder. Am J Psychiatry (2006) 163(5):822–6. doi: 10.1176/ajp.2006.163.5.822
97. Newton-Howes G, Clark LA, Chanen A. Personality disorder across the life course. Lancet (2015) 385(9969):727–34. doi: 10.1016/S0140-6736(14)61283-6
98. Zanarini MC, Temes CM, Ivey AM, Cohn DM, Conkey LC, Frankenburg FR, et al. The 10-year course of adult aggression toward others in patients with borderline personality disorder and axis II comparison subjects. Psychiatr Res (2017) 252:134–8. doi: 10.1016/j.psychres.2017.02.054
99. Winsper C, Marwaha S, Lereya ST, Thompson A, Eyden J, Singh SP. Clinical and psychosocial outcomes of borderline personality disorder in childhood and adolescence: a systematic review. Psychol Med (2015) 45(11):2237–51. doi: 10.1017/S0033291715000318
100. Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: prognosis for functioning over 20 years. J Child Psychol Psychiatry (2008) 49(9):933–41. doi: 10.1111/j.1469-7610.2008.01930.x
101. Crawford TN, Cohen P, First MB, Skodol AE, Johnson JG, Kasen S. Comorbid Axis I and Axis II disorders in early adolescence: outcomes 20 years later. Arch Gen Psychiatry (2008) 65(6):641–8. doi: 10.1001/archpsyc.65.6.641
102. Biskin RS, Paris J, Renaud J, Raz A, Zelkowitz P. Outcomes in women diagnosed with borderline personality disorder in adolescence. J Can Acad Child Adolesc Psychiatry (2011) 20(3):168–74.
103. Stone MH. Long-term course of borderline personality disorder. Psychodyn Psychiatry (2016) 44(3):449–74. doi: 10.1521/pdps.2016.44.3.449
104. Zanarini MC, Frankenburg FR, Reich DB, Wedig MM, Conkey LC, Fitzmaurice GM. Prediction of time-to-attainment of recovery for borderline patients followed prospectively for 16 years. Acta Psychiatr Scand (2014) 130(3):205–13. doi: 10.1111/acps.12255
105. Stepp SD, Keenan K, Hipwell AE, Krueger RF. The impact of childhood temperament on the development of borderline personality disorder symptoms over the course of adolescence. Borderline Pers Disord Emot Dysregul (2014) 1(1): 18. doi: 10.1186/2051-6673-1-18
106. National Institute for Health and Clinical Excellence (NICE). Borderline personality disorder: treatment and management. Clinical Guideline 78 . London, UK: National Collaborating Centre for Mental Health (2009). Available from: www.guidance.nice.org.uk/CG78
Google Scholar
107. Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. J Abnorm Child Psychol (2012) 40(1):35–44. doi: 10.1007/s10802-011-9558-7
108. Bozzatello P, Morese R, Valentini MC, Rocca P, Bosco F, Bellino S. Autobiographical memories, identity disturbance and brain functioning in patients with borderline personality disorder: an fMRI study. Heliyon (2019) 5(3):1–21. doi: 10.1016/j.heliyon.2019.e01323
Keywords: borderline personality disorder, prodromal factors, early symptoms, childhood, adolescence, outcome
Citation: Bozzatello P, Bellino S, Bosia M and Rocca P (2019) Early Detection and Outcome in Borderline Personality Disorder. Front. Psychiatry 10:710. doi: 10.3389/fpsyt.2019.00710
Received: 07 January 2019; Accepted: 04 September 2019; Published: 09 October 2019.
Reviewed by:
Copyright © 2019 Bozzatello, Bellino, Bosia and Rocca. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvio Bellino, c2lsdmlvLmJlbGxpbm9AdW5pdG8uaXQ=
† These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Diagnosing borderline personality disorder
Robert s biskin , md, joel paris , md.
- Author information
- Copyright and License information
Correspondence to: Robert S. Biskin, [email protected]
Borderline personality disorder can be a difficult diagnosis because of similarities to other conditions, particularly mood disorders. It is a common presentation in both psychiatric and general practice, with accurately diagnosed cases seen in 10% of psychiatric outpatients, 20% of psychiatric inpatients 1 , 2 and 6% of family medicine patients. 3 These values are higher than would be expected given a prevalence of about 1% in the general population. 4 Women account for 70% of patients with this disorder in clinical settings, 5 and the most common age at first presentation is in late adolescence. 6 Unfortunately, a large proportion of patients with the disorder are not identified in practice. 3
Patients with borderline personality disorder are frequently encountered in the emergency department, where they present following threatened suicide or a suicide attempt. More than 500 000 such visits to emergency departments occur each year in the United States. 7 The incidence of suicide attempts among patients with borderline personality disorder is highest among those in their twenties, but mortality peaks in the thirties, with a 10% lifetime rate of completed suicide. 8
Retrospective studies have shown that symptoms resolve over time, with 75% of patients at 15-year follow-up and 92% of patients at 27-year follow-up no longer having the disorder. 8 , 9 One large, well-conducted 10-year prospective study found that 93% of those with borderline personality disorder had at least a 2-year period of remission, but only 50% also attained good psychosocial functioning. 10
In this article, we focus on the current diagnostic criteria for borderline personality disorder, as presented in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), 11 and how these criteria can be used to differentiate it from other disorders that may share symptoms. A summary of the evidence used in this review is found in Box 1 . We based our review primarily on findings from a relatively small body of experimental studies that used the very similar DSM-III 12 and DSM-IV 13 definitions of borderline personality disorder and its symptoms. Recent research, which was the focus of our review, was generally of high quality and used sophisticated assessment and measurement strategies to differentiate the disorder from other psychiatric disorders.
Box 1: Evidence used in this review.
We searched MEDLINE for articles published from 1950 to 2012 using the search terms “borderline personality disorder” and “diagnosis” or “diagnosis, differential.” Of the 393 studies identified, we excluded case reports, commentaries, editorials, letters and reviews, which left 210 articles in English. After reviewing the titles, we selected the abstracts of articles that focused on diagnostic issues. We retrieved the full-text versions if they were relevant to general clinical practice. The most recent articles were preferred for inclusion, particularly those that reflected the current diagnostic criteria and were applicable across multiple clinical settings. When necessary, specific diagnostic criteria, such as emptiness and affective instability, were used as search terms to provide further detail regarding the differential diagnosis.
What is the origin of the term “borderline personality disorder”?
The term “borderline” was first described by the psychoanalyst Adolf Stern in 1938. 14 He used it to refer to a group of patients whose conditions worsened during therapy and who showed masochistic behaviour and psychic rigidity, indicating a protective mechanism against any perceived changes in the environment or within the individual. The term was later expanded in the late 1960s and 1970s by Otto Kernberg; 15 this diagnosis was used in empirical studies conducted by Grinker and Werble. 16 Gunderson and Singer reviewed the literature and listed several features that identify borderline personality disorder, 17 and a diagnostic interview based on these features was later developed by Gunderson and colleagues. 18 The diagnosis was included in the DSM-III 12 and was slightly revised in the DSM-IV, 13 with the addition of a ninth criterion for cognitive symptoms, but both sets of criteria were based primarily on clinical experience and the work of Gunderson and Singer. 17 The definition in the DSM-IV-TR is unchanged, 11 although important modifications have been proposed for DSM-5. 19 In particular, the diagnostic system for personality disorders will become a hybrid model, with both categorical diagnoses, including borderline personality disorder, and a dimensional system based on personality traits. The proposed categorical diagnosis of borderline personality disorder includes traits and symptoms that are generally similar to those in previous versions of the DSM.
The validity of the current criteria for borderline personality disorder shares problems with other psychiatric disorders: namely, the absence of biological markers, unclear delimitation from other disorders, and a wide variety of combinations of symptoms that could lead to heterogeneity. Currently, the diagnostic criteria in the DSM-IV-TR remain the standard.
How is borderline personality disorder diagnosed?
The diagnosis is based on symptoms that have been present since adolescence or early adulthood and appear in multiple contexts. 11 There are no laboratory or imaging tests that can help with the diagnosis. 20 A number of structured and semistructured interviews can assist in making the diagnosis, although they often require specialized training to administer. 21 , 22 The Diagnostic Interview for Borderlines – Revised 21 is a validated and frequently used tool that is generally considered the “gold standard”; however, it can take 30–60 minutes to administer. Several self-report measures have been developed within the past decade 23 – 26 but are rarely used in routine clinical practice. One commonly used self-report questionnaire for mood disorders — the Mood Disorder Questionnaire — frequently misdiagnoses borderline personality disorder as bipolar disorder. 27
When interviewing patients, different domains of symptoms must be explored. Symptoms in borderline personality disorder occur in 4 domains: affectivity, interpersonal functioning, impulse control and cognitive. 11 The diagnosis requires that at least 5 of 9 specific criteria be met ( Box 2 ). 11
Box 2: Diagnostic criteria of borderline personality disorder * .
A pervasive pattern of instability of interpersonal relationships, self-image and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by 5 (or more) of the following:
Frantic efforts to avoid real or imagined abandonment. Note: Do not include suicidal or self-mutilating behaviour covered in criterion 5.
A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
Identity disturbance: markedly and persistently unstable self-image or sense of self.
Impulsivity in at least 2 areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating). Note: Do not include suicidal or self-mutilating behaviour covered in criterion 5.
Recurrent suicidal behaviour, gestures or threats, or self-mutilating behaviour.
Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability or anxiety usually lasting a few hours and only rarely more than a few days).
Chronic feelings of emptiness.
Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
Transient, stress-related paranoid ideation or severe dissociative symptoms.
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision . 11 Copyright © 2000 American Psychiatric Association.
Affective symptoms
The first affective criterion is the presence of “affective instability due to a marked reactivity of mood … that lasts hours to rarely more than a few days.” 11 These frequent mood changes may appear to overlap with bipolar disorder, but there are several clear distinctions. First, the duration of the fluctuations is shorter than in bipolar disorder. In bipolar disorder, mood changes must remain consistent and persist for at least 4 days to meet criteria for a hypomanic episode and 7 days for a manic episode. 11
A second difference is the persistence of affective lability throughout life, rather than during a discrete mood episode. 28 Moreover, symptoms of borderline personality disorder gradually improve with time. 4 , 29 – 31 In contrast, bipolar disorder has discrete periods (lasting on average 3 months) for both mania and depression that cause patients to present and function distinctly differently from their baseline, and these episodes can occur at any point during a patient’s life. 32
The third difference is reactivity of mood. The mood symptoms of patients with borderline personality disorder are triggered by external events 33 and are particularly sensitive to perceived rejection, failure and abandonment. 34 Moods usually shift between depression and anger, and euphoria is transient. Shifts between depression and euphoria are more frequently seen in bipolar disorder. 35 Most of the data on affective lability are derived from ecological momentary assessment studies, in which patients are asked to record mood fluctuations and psychosocial stressors several times each day. This technique provides results that are consistent, different and more valid than when patients are asked at a later point to recall their experiences. 36
Several characteristics may help distinguish mood fluctuations in patients with borderline personality disorder from those in healthy controls. Several studies suggest that negative emotions may persist for longer and be more intense in patients with the disorder than in healthy controls, although this is not true for positive emotions. 34 , 37 , 38 A second discriminating characteristic is the quality of mood reported by patients with the disorder. Several high-quality observational studies that used ecological momentary assessment found that patients with borderline personality disorder described continuous dysphoria, high emotional variability 33 , 39 and increased hostility 40 compared with healthy controls.
Inappropriate and intense anger is the next affective symptom of borderline personality disorder and is related to affective instability, as described earlier. The final affective symptom is a chronic feeling of emptiness. This experience is hard to define and lacks specificity for the diagnosis compared with other diagnostic criteria. 41 However, patients with the disorder have described it as feeling as if “something is missing,” and it overlaps with hopelessness, isolation and loneliness, as well as some symptoms of depression. 42 One small study found that symptoms of emptiness, along with self-condemnation, hopelessness and other symptoms of the disorder, including fear of abandonment and self-destructiveness, help distinguish the disorder from major depression. 43
Impulsive symptoms
The impulsive symptoms of borderline personality disorder may be more recognizable to clinicians, but they can still pose diagnostic challenges. Patients with recurrent suicide attempts or threats or episodes of self-harm are commonly seen in the emergency department and in psychiatric assessments. 7 Between 60% and 78% of patients with the disorder have shown suicidal behaviours, with more than 90% engaging in self-harm. 44 , 45 Persistent cutting as a way of regulating emotions is a characteristic feature of the disorder, as are recurrent overdoses related to stressful events. 46 Recurrent presentation to the emergency department because of suicidality is suggestive of the diagnosis, with almost half of such patients meeting the diagnostic criteria for borderline personality disorder. 47 , 48
Impulsivity and self-destructiveness in borderline personality disorder encompass many other behaviours, including gambling, spending, binge eating and sexual promiscuity. Substance abuse is also frequent: alcohol and substance abuse or dependence are seen in more than 50% of patients with the disorder. 49 The combination of substance use and borderline personality disorder is associated with an increased risk of completed suicide. 50
Interpersonal symptoms
A pattern of unstable relationships, marked by extremes of idealization and devaluation, is one of the most important symptoms in making an accurate diagnosis of borderline personality disorder, with studies reporting a sensitivity of 74% and a specificity of 87%. 41 , 51 Because of this interpersonal instability, less than half of women with the disorder marry, and even less have children. 29 Patients with the disorder also make frantic efforts to avoid abandonment. Clinical experience suggests that, over time, some patients react to this fear by becoming socially isolated to protect themselves from potential abandonment.
Identity disturbance is the second interpersonal symptom. This symptom has not been clearly defined, but it generally refers to frequent and suddenly changing goals, beliefs, vocational aspirations and sexual identity, as well as a painful sense of incoherence. Patients may also feel as if they are assuming the identity of other people to whom they are close. 5 The identity disturbance seen in this disorder should be differentiated from the normal identity issues one sees in adolescents. Being unable to define an identity on one’s own and instead being dependent on interpersonal relationships to define one’s identity, as well as frequent fluctuations or a sense of incoherence in one’s identity, are more strongly associated with borderline personality disorder than with typical adolescent identity issues. 52
Cognitive symptoms
Few studies of cognitive symptoms in borderline personality disorder have been conducted. What is known is that about 40%–50% of patients with the disorder have brief periods of psychotic symptoms or dissociation. 53 Typical symptoms include paranoid thoughts and auditory hallucinations, but their course is much shorter than in schizophrenia, often lasting only hours to days, and the presence of symptoms is related to stressors. 20 Compared with psychotic experiences of patients with schizophrenia, those of patients with borderline personality disorder are much more likely to be short, circumscribed, and either based in reality or totally fantastic. 53
Other cognitive features that are common include depersonalization (i.e, the sensation that a person’s body or self is unreal or altered in a strange way), derealization (i.e., the experience that the external world is bizarre and unreal) and illusions, which are misperceptions of existing stimuli. 5 These symptoms can also occur in posttraumatic stress disorder, 11 but the presence of suicide proneness, impulsivity, disturbed relationships and affective dysregulation are all more commonly seen in borderline personality disorder. 54
What are the challenges in making the diagnosis?
The current diagnostic criteria for borderline personality disorder allow for 256 different combinations of symptoms that could lead to a diagnosis. Clinicians thus may find it challenging to make a diagnosis of borderline personality disorder. Because of their limited time to spend with patients, clinicians can look for several key factors to help them decide whether further assessment for the disorder is necessary.
The most important factor is whether the difficulties have been long standing or, for adolescents, present for at least 1 year. 11 If there is a sudden change in functioning or new symptoms, a diagnosis of borderline personality disorder is less likely according to the DSM-IV-TR definition. 11
Having difficulties in multiple areas is another important factor. 11 , 21 For example, suicidality or self-harm without problems with mood or relationships is less likely to be borderline personality disorder, whereas a history of suicide attempts along with impulsive substance use and problems with chronic feelings of emptiness and anger is more suggestive of a diagnosis.
If the diagnosis of borderline personality disorder is not made, an affected person may end up with several diagnoses of comorbid disorders, none of which responds to common treatments. For example, patients who have major depressive disorder and comorbid borderline personality disorder generally do not respond as well to antidepressant medications as patients do who have major depressive disorder alone. 55
How should patients be informed of their diagnosis?
Once a diagnosis of borderline personality disorder has been established, it is important to inform the patient of the diagnosis and discuss the implications for treatment options and outcomes. There is no evidence to indicate that informing patients of the diagnosis causes problems, so it is unfortunate that this important step is often omitted. 56
When informing a patient about a suspected diagnosis of borderline personality disorder, clinical experience suggests that it is helpful to show the patient the list of diagnostic criteria and explain why the diagnosis is being considered. Educating patients about the increasing number of specific treatments and the good prognosis with gradually resolving symptoms can also help reduce their anxiety about a diagnosis that is highly stigmatized in the medical system and the general population. Even a single psychoeducation session could help to reduce symptoms, as was found in a randomized trial in which 30 of 50 late adolescent women found to have borderline personality disorder were randomly assigned to attend such a session within a week after being told about their diagnosis. 57 Patients can also be directed to specific resources that can provide more information ( Box 3 ).
Box 3: Resources for patients and clinicians.
For patients
National Institute of Mental Health: www.nimh.nih.gov/health/topics/borderline-personality-disorder/index.shtml
Borderline Personality Disorder Resource Center: http://bpdresourcecenter.org/
National Education Alliance for Borderline Personality Disorder: www.borderlinepersonalitydisorder.com/index.html
Chapman AL, Gratz KL. The borderline personality disorder survival guide: everything you need to know about living with BPD . Oakland (CA): New Harbinger Publications; 2007.
For clinicians
Behavioural Tech, LLC (for clinicians interested in dialectical behaviour therapy): www.behavioraltech.org/index.cfm
Paris J. Treatment of borderline personality disorder: a guide to evidence-based practice . New York (NY): Guilford Press; 2008.
Gunderson JG, Links PS. Borderline personality disorder: a clinical guide . Washington (DC): American Psychiatric Publishing; 2008.
Beyond the ethical implications of informing patients of their diagnosis, patients benefit from improved understanding about their disorder and often feel as if the clinical picture “finally makes sense.” 20 , 58 Informing patients may also help to prevent misunderstandings about the diagnosis and to avoid improper treatments in the future.
Overlap of symptoms with those of other psychiatric disorders makes diagnosis of borderline personality disorder a challenge. Careful evaluation can usually clarify the clinical picture. Box 4 gives an example of how the diagnostic criteria can be applied in practice.
Box 4: Applying the results of this review in clinical practice (fictional case).
A 39-year-old woman with a long psychiatric history presented for assessment in a specialized personality disorder clinic. She was first seen at age 19 with depression in the context of an abusive relationship. At the time, she was prescribed an antidepressant and gradually felt somewhat better, but she continued to have problems with mood fluctuations. The patient was seen again at age 25 for elevated mood accompanied by decreased sleep and increased energy in the context of an exciting new relationship. Although she reported that these symptoms were present “all the time,” her diagnosis was changed to bipolar disorder and the antidepressant switched to lithium. Her mood quickly became depressed, coinciding with the breakup of the relationship. Three months later, the patient became increasingly isolated with anxiety about further “emotional trauma” induced by her last breakup. After a particularly stressful day at work, she threatened to overdose on medications, because “the voice of my dead grandmother told me to.” These symptoms were new, and the patient also reported feeling as if she was not real and that she was in a television program. The diagnosis was revised to schizoaffective disorder, and the patient was admitted to hospital and given antipsychotic drug treatment. The psychotic symptoms resolved in a matter of days, but the patient remained suicidal with depression that fluctuated with episodes of anger. A pattern of impulsive suicide attempts, psychotic symptoms and psychiatric admissions persisted for the next 10 years, despite numerous medications. Throughout this period, the patient continued to attend school and began a job as a child care worker in a special education environment.
During the current assessment at the clinic, the patient reported that her elevated mood was present only for several hours at a time. During these periods, she experienced symptoms of irritability and affective lability that remained unchanged from baseline, which indicated that she did not experience discrete hypomanic episodes. The patient reported that, even during periods of elevated mood, she was able to attend work and concentrate. These mood fluctuations were usually brought on by conflicts with partners or family. When at work or in low stress situations, she would feel euthymic. Her psychotic symptoms would also occur during episodes of high stress and persisted only for several hours. At times, symptoms would resolve within days, even without seeking medical treatment. With a revised diagnosis of borderline personality disorder, the patient began a long-term program of specialized individual and group psychotherapy, during which most of her medications were gradually removed. This focused approach to treatment led to a decrease in symptoms and improvements in her interpersonal relationships.
Gaps in knowledge
Accurate diagnosis of borderline personality disorder remains challenging. It is easy to miss the forest for the trees by identifying a single symptom and making an incorrect diagnosis based on that symptom alone. Borderline personality disorder is a clinical diagnosis, with no supporting laboratory or imaging tests. Even the core pathological features remain in debate, 46 , 59 but there is a broad consensus supporting the current criteria.
One area that is receiving increasing attention is the presentation, course and treatment of the disorder in adolescents. 60 – 62 Research in this area will allow for earlier diagnosis and treatment, which may lead to improved long-term outcomes.
Another major issue is how the change to a trait-based diagnostic system in the upcoming DSM-5 will affect the diagnosis of borderline personality disorder, with debate over how clinically useful such a system will be. 63 , 64
Once a diagnosis is made and the patient informed, a discussion about treatment can follow. In the past, treatment of borderline personality disorder was considered challenging, but some interventions have been developed over the past 2 decades that have dramatically changed the lives of patients with this disorder. In a related article in CMAJ , 65 we will review the literature on the treatment of borderline personality disorder and provide some general suggestions on how to manage patients with the disorder.
Borderline personality disorder is a clinically important psychiatric disorder that is distinct from major depressive disorder, bipolar disorder and posttraumatic stress disorder, despite overlapping symptoms.
Symptoms of borderline personality disorder manifest in problems in affectivity, interpersonal functioning, impulse control and cognition.
Borderline personality disorder can be distinguished from other disorders if a number of these symptoms occur together.
When borderline personality disorder is recognized, patients should be informed of the diagnosis, and the treatment options and outcomes discussed.
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Robert Biskin drafted the manuscript and conducted the literature review. Joel Paris supervised the process and rewrote and edited sections of the manuscript. Both authors approved the final version submitted for publication.
- 1. Widiger TA, Weissman MM. Epidemiology of borderline personality disorder. Hosp Community Psychiatry 1991;42:1015–21 [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Zimmerman M, Rothschild L, Chelminski I. The prevalence of DSM-IV personality disorders in psychiatric outpatients. Am J Psychiatry 2005;162:1911–8 [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Gross R, Olfson M, Gameroff M, et al. Borderline personality disorder in primary care. Arch Intern Med 2002;162:53–60 [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007;62:553–64 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Gunderson JG, Links PS. Borderline personality disorder: a clinical guide. 2nd ed Washington (DC): American Psychiatric Publishing; 2008. p. 350 [ Google Scholar ]
- 6. Zanarini MC, Frankenburg FR, Khera GS, et al. Treatment histories of borderline inpatients. Compr Psychiatry 2001;42: 144–50 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. The Surgeon General’s call to action to prevent suicide. Washington (DC): United States Public Health Service; 1999 [ Google Scholar ]
- 8. Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry 2001;42:482–7 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Paris J, Brown R, Nowlis D. Long-term follow-up of borderline patients in a general hospital. Compr Psychiatry 1987;28:530–5 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Zanarini MC, Frankenburg FR, Reich DB, et al. Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10-year prospective follow-up study. Am J Psychiatry 2010;167:663–7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. American Psychiatric Association Diagnostic and statistical manual of mental disorders. Fourth edition. Text revision. Washington (DC): The Association; 2000. p. 943 [ Google Scholar ]
- 12. American Psychiatric Association Diagnostic and statistical manual of mental disorders. 3rd ed Washington (DC): The Association; 1980. p. 494 [ Google Scholar ]
- 13. American Psychiatric Association Diagnostic and statistical manual of mental disorders. 4th ed Washington (DC): The Association; 1994. p. 886 [ Google Scholar ]
- 14. Stern A. Psychoanalytic Investigation of and therapy in the border line group of neuroses. Psychoanal Q 1938;7:467–89 [ Google Scholar ]
- 15. Kernberg OF. A psychoanalytic classification of character pathology. J Am Psychoanal Assoc 1970;18:800–22 [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Grinker RR, Werble B. The borderline patient. New York (NY): Jason Aronson Inc.; 1977. p. 226 [ Google Scholar ]
- 17. Gunderson JG, Singer MT. Defining borderline patients: an overview. Am J Psychiatry 1975;132:1–10 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Gunderson JG, Kolb JE, Austin V. The diagnostic interview for borderline patients. Am J Psychiatry 1981;138:896–903 [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Skodol AE, Bender DS, Morey LC, et al. Personality disorder types proposed for DSM-5. J Pers Disord 2011;25:136–69 [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Paris J. Treatment of borderline personality disorder: a guide to evidence-based practice. New York (NY): Guilford Press; 2008. p. 260 [ Google Scholar ]
- 21. Zanarini MC, Gunderson JG, Frankenburg FR, et al. Discriminating BPD from other axis II disorders. J Pers Disord 1989;3:10–8 [ Google Scholar ]
- 22. First MB. User’s guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II. Washington (DC): American Psychiatric Press; 1997. p. 91 [ Google Scholar ]
- 23. Poreh AM, Rawlings D, Claridge G, et al. The BPQ: a scale for the assessment of borderline personality based on DSM-IV criteria. J Pers Disord 2006;20:247–60 [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Arntz A, van den Hoorn M, Cornelis J, et al. Reliability and validity of the Borderline Personality Disorder Severity Index. J Pers Disord 2003;17:45–59 [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Zanarini MC, Vujanovic AA, Parachini EA, et al. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD). J Pers Disord 2003;17:568–73 [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Zanarini MC, Vujanovic AA, Parachini EA, et al. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology [published erratum in J Pers Disord 2003;17:370]. J Pers Disord 2003;17:233–42 [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Zimmerman M, Galione JN, Ruggero CJ, et al. Screening for bipolar disorder and finding borderline personality disorder. J Clin Psychiatry 2010;71:1212–7 [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Grilo CM, McGlashan TH, Skodol AE. Stability and course of personality disorders: the need to consider comorbidities and continuities between axis I psychiatric disorders and axis II personality disorders. Psychiatr Q 2000;71:291–307 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Paris J. Personality disorders over time: precursors, course and outcome. J Pers Disord 2003;17:479–88 [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Tracie Shea M, Edelen MO, Pinto A, et al. Improvement in borderline personality disorder in relationship to age. Acta Psychiatr Scand 2009;119:143–8 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Zanarini MC, Frankenburg FR, Reich DB, et al. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am J Psychiatry 2007;164:929–35 [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Goodwin FK, Jamison KR, Ghaemi SN. Manic–depressive illness: bipolar disorders and recurrent depression. 2nd ed New York (NY): Oxford University Press; 2007. p. 1262 [ Google Scholar ]
- 33. Nica EI, Links PS. Affective instability in borderline personality disorder: experience sampling findings. Curr Psychiatry Rep 2009;11:74–81 [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Stiglmayr CE, Shapiro DA, Stieglitz RD, et al. Experience of aversive tension and dissociation in female patients with borderline personality disorder: a controlled study. J Psychiatr Res 2001; 35:111–8 [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res 2001;35:307–12 [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Solhan MB, Trull TJ, Jahng S, et al. Clinical assessment of affective instability: comparing EMA indices, questionnaire reports, and retrospective recall. Psychol Assess 2009;21:425–36 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Stiglmayr CE, Grathwol T, Linehan MM, et al. Aversive tension in patients with borderline personality disorder: a computer-based controlled field study. Acta Psychiatr Scand 2005;111:372–9 [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Zeigler-Hill V, Abraham J. Borderline personality features: instability of self-esteem and affect. J Soc Clin Psychol 2006;25:668–87 [ Google Scholar ]
- 39. Russell JJ, Moskowitz DS, Zuroff DC, et al. Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. J Abnorm Psychol 2007;116:578–88 [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Trull TJ, Solhan MB, Tragesser SL, et al. Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. J Abnorm Psychol 2008;117:647–61 [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Johansen M, Karterud S, Pedersen G, et al. An investigation of the prototype validity of the borderline DSM-IV construct. Acta Psychiatr Scand 2004;109:289–98 [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Klonsky ED. What is emptiness? Clarifying the 7th criterion for borderline personality disorder. J Pers Disord 2008;22:418–26 [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Rogers JH, Widiger TA, Krupp A. Aspects of depression associated with borderline personality disorder. Am J Psychiatry 1995; 152:268–70 [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Zaheer J, Links PS, Liu E. Assessment and emergency management of suicidality in personality disorders. Psychiatr Clin North Am 2008;31:527–43 [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Zanarini MC, Frankenburg FR, Ridolfi ME, et al. Reported childhood onset of self-mutilation among borderline patients. J Pers Disord 2006;20:9–15 [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York (NY): Guilford Press; 1993. p. 558 [ Google Scholar ]
- 47. Bongar B, Peterson LG, Golann S, et al. Self-mutilation and the chronically suicidal patient: an examination of the frequent visitor to the psychiatric emergency room. Ann Clin Psychiatry 1990;2:217–22 [ Google Scholar ]
- 48. Forman EM, Berk MS, Henriques GR, et al. History of multiple suicide attempts as a behavioral marker of severe psychopathology. Am J Psychiatry 2004;161:437–43 [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. McGlashan TH, Grilo CM, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: baseline axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand 2000;102: 256–64 [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. McGirr A, Paris J, Lesage A, et al. Risk factors for suicide completion in borderline personality disorder: a case–control study of cluster B comorbidity and impulsive aggression. J Clin Psychiatry 2007;68:721–9 [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Fossati A, Maffei C, Bagnato M, et al. Latent structure analysis of DSM-IV borderline personality disorder criteria. Compr Psychiatry 1999;40:72–9 [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Westen D, Betan E, Defife JA. Identity disturbance in adolescence: associations with borderline personality disorder. Dev Psychopathol 2011;23:305–13 [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Zanarini MC, Gunderson JG, Frankenburg FR. Cognitive features of borderline personality disorder. Am J Psychiatry 1990; 147:57–63 [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Zlotnick C, Johnson DM, Yen S, et al. Clinical features and impairment in women with borderline personality disorder (BPD) with posttraumatic stress disorder (PTSD), BPD without PTSD, and other personality disorders with PTSD. J Nerv Ment Dis 2003;191:706–13 [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br J Psychiatry 2006;188:13–20 [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. McDonald-Scott P, Machizawa S, Satoh H. Diagnostic disclosure: a tale in two cultures. Psychol Med 1992;22:147–57 [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord 2008;22:284–90 [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Lequesne ER, Hersh RG. Disclosure of a diagnosis of borderline personality disorder. J Psychiatr Pract 2004;10:170–6 [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Bateman A, Fonagy P. Psychotherapy for borderline personality disorder: mentalization-based treatment. Oxford (UK): Oxford University Press; 2004. p. 381 [ Google Scholar ]
- 60. Biskin RS, Paris J, Renaud J, et al. Outcomes in women diagnosed with borderline personality disorder in adolescence. J Can Acad Child Adolesc Psychiatry 2011;20:168–74 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Stepp SD, Pilkonis PA, Hipwell AE, et al. Stability of borderline personality disorder features in girls. J Pers Disord 2010;24:460–72 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Chanen AM, McCutcheon LK, Germano D, et al. The HYPE Clinic: an early intervention service for borderline personality disorder. J Psychiatr Pract 2009;15:163–72 [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Gunderson JG. Revising the borderline diagnosis for DSM-V: an alternative proposal. J Pers Disord 2010;24:694–708 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 64. Hopwood CJ, Malone JC, Ansell EB, et al. Personality assessment in DSM-5: empirical support for rating severity, style, and traits. J Pers Disord. 2011;25:305–20 [ DOI ] [ PubMed ] [ Google Scholar ]
- 65. Biskin RS, Paris J. Management of borderline personality disorder. CMAJ 2012; Oct. 1 [Epub ahead of print]. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (101.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Open access
- Published: 15 February 2023
Developmental predictors of young adult borderline personality disorder: a prospective, longitudinal study of females with and without childhood ADHD
- Sinclaire M. O’Grady 1 &
- Stephen P. Hinshaw 1 , 2
BMC Psychiatry volume 23 , Article number: 106 ( 2023 ) Cite this article
8758 Accesses
5 Citations
10 Altmetric
Metrics details
Research on the precursors of borderline personality disorder (BPD) reveals numerous child and adolescent risk factors, with impulsivity and trauma among the most salient. Yet few prospective longitudinal studies have examined pathways to BPD, particularly with inclusion of multiple risk domains.
We examined theory-informed predictors of young-adult BPD (a) diagnosis and (b) dimensional features from childhood and late adolescence via a diverse (47% non-white) sample of females with ( n = 140) and without ( n = 88) carefully diagnosed childhood attention-deficit hyperactivity disorder (ADHD).
After adjustment for key covariates, low levels of objectively measured executive functioning in childhood predicted young adult BPD diagnostic status, as did a cumulative history of childhood adverse experiences/trauma. Additionally, both childhood hyperactivity/impulsivity and childhood adverse experiences/trauma predicted young adult BPD dimensional features. Regarding late-adolescent predictors, no significant predictors emerged regarding BPD diagnosis, but internalizing and externalizing symptoms were each significant predictors of BPD dimensional features. Exploratory moderator analyses revealed that predictions to BPD dimensional features from low executive functioning were heightened in the presence of low socioeconomic status.
Conclusions
Given our sample size, caution is needed when drawing implications. Possible future directions include focus on preventive interventions in populations with enhanced risk for BPD, particularly those focused on improving executive functioning skills and reducing risk for trauma (and its manifestations). Replication is required, as are sensitive measures of early emotional invalidation and extensions to male samples.
Peer Review reports
Borderline personality disorder (BPD) is a persistent and highly impairing condition characterized by intense and pervasive dysregulation of emotion, behavior, and cognition, and a pattern of highly unstable interpersonal relationships [ 1 ]. Individuals with BPD are at extremely high risk for suicide: Up to 10% of individuals with BPD die by suicide each year, 50 times higher than the rate in the general population [ 2 , 3 ]. BPD is also associated with significant personal (i.e., severe psychosocial impairment) and economic/public health (i.e., high rates of underemployment and increased disability) consequences. In fact, although individuals with BPD comprise 1–2% of the general population [ 4 ], they have extremely high rates of health service use, representing up to 20% of individuals receiving inpatient psychiatric treatment and 10% receiving outpatient psychiatric care [ 5 ]. Evidence-based psychological treatments (e.g., Dialectical Behavior Therapy [DBT]) exist for BPD, with strong evidence for efficacy [ 6 ]. Yet they are resource-intensive, with limited availability of expert providers.
Given the high morbidity, mortality, and public health consequences of BPD, an urgent need exists to identify individuals at risk for its development. Relevant research is accumulating. A leading model is Linehan’s Biosocial Theory, which proposes that BPD emerges from transactions between (a) biological vulnerabilities linked with both impulsivity and emotional sensitivity and (b) specific environmental influences such as social invalidation, adversity, or trauma [ 1 , 7 ]. Across development, such combinations give rise to increasingly extreme emotional, behavioral, cognitive, and interpersonal dysregulation for vulnerable individuals. Although empirical research has generated numerous potential risk factors for BPD [ 8 , 9 ], relatively few studies have examined longitudinal pathways to BPD. Identification of such would help strengthen theoretical approaches to the development of BPD. In particular, few studies have examined childhood risk factors for BPD in prospective designs [ 10 ]. Indeed, a 2016 systematic review of risk factors for BPD revealed that risk factors were assessed mainly during early adolescence ( M age = 13 years), highlighting the need for further investigation of childhood variables and processes [ 9 ]. Such studies could further inform leading theories [ 1 , 11 ] regarding heightened periods of risk (and areas for intervention). In the present investigation, we examine both child and late-adolescent risk factors for later BPD.
Developmental risk factors for BPD
Adhd symptoms.
Impulsivity is a key feature in both the development and presentation of BPD [ 1 ]. It is also a core symptom of attention-deficit hyperactivity disorder (ADHD). In fact, several studies have reported high comorbidity between BPD and ADHD [ 12 , 13 ]. In a large national study of 34,000 adults in the United States, among adults with ADHD the lifetime comorbidity with BPD was 33.7% [ 14 ]. Comorbid ADHD and BPD is a particularly impairing combination [ 12 ]. As for childhood ADHD in relation to adult BPD, most prior research has involved retrospective reports of symptoms. Here, 50–60% of adults with BPD endorsed high levels of ADHD symptoms in childhood [ 15 ]. Philipsen et al. [ 16 ] reported estimates of ADHD among adult women with BPD to be especially high during childhood (41.5%) as compared to adulthood (16.1%). Severity of childhood ADHD symptoms is also associated with higher frequency of personality disorder diagnoses, including BPD, by adulthood [ 17 ].
Hypothesized mechanisms linking ADHD and BPD focus on the interaction, across development, between early impulsivity (a highly heritable trait) and emotion dysregulation, the combination of which, in turn, is shaped by adverse socialization processes (e.g., maltreatment, family reinforcement of emotional lability) [ 11 ]. Proposed neurobiological mechanisms focus on dysfunction in the prefrontal cortex, which is also implicated in emotion regulatory capacities [ 11 , 18 ]. Essentially, early ADHD is hypothesized to confer risk for later BPD because of its associated behavioral dysregulation, promoting environmental reinforcement of maladaptive behaviors and often leading to a pervasive and difficult-to-treat cycle of dysregulation.
As noted above, however, few prospective studies have examined the link between childhood ADHD and later BPD. Notable exceptions (see [ 19 , 20 , 21 ]) reveal that childhood ADHD predicts personality disorders, including BPD, later in life. In a follow-up investigation of “hyperactive” children in young adulthood, Fischer et al. [ 22 ] found that 14% of hyperactive participants met criteria for BPD compared to 3% of their comparison group. Miller et al. [ 13 ] found that among a group with childhood ADHD, 13.5% were diagnosed with BPD in adolescence compared to 1.2% in their comparison group. Furthermore, in the Pittsburgh Girls Study, Stepp et al. [ 18 ] found that high levels of ADHD symptoms during childhood predicted BPD in adolescence (see also [ 23 ] for parallel findings in males). Using latent-class analysis, Thatcher et al. [ 24 ] found that the presence of ADHD symptoms in adolescents, along with substance use disorders, predicted more severe BPD symptoms at young-adult follow-up.
The majority of relevant research has focused on the categorical diagnosis of ADHD rather than the core ADHD dimensions of (a) hyperactivity/impulsivity and (b) inattention. Exceptions include Carlson et al. [ 25 ], who reported data from a prospective, longitudinal study. Teacher-rated severity of both attentional disturbance and behavioral instability (including impulsivity) at age 12 was predictive of adult BPD. This finding was recently replicated by Beeney et al. [ 8 ] in a prospective study of females. Here, parent- and child-reported severity of hyperactivity, impulsivity, and inattention at ages 14–15 predicted BPD at ages 16–18. In a prospective study in twins, maternal- and teacher-rated symptoms of impulsivity at age 5 were related to borderline symptoms at age 12 [ 26 ]. Finally, a recent national, prospective longitudinal study of twins in Sweden found that the association between childhood ADHD symptoms, assessed at age 9 or 12, and adult BPD was primarily driven by impulsivity as opposed to inattention or hyperactivity [ 27 ].
Some adult research has examined presentations (or “types”) of ADHD as related to BPD. Among adults with ADHD, one study reported a higher prevalence rate of comorbid BPD in the Combined presentation of ADHD (ADHD-C; 24%), for which hyperactivity/impulsivity and inattention are key components, compared to comorbid BPD and the Inattentive presentation (ADHD-I; 10%) [ 28 ]. Using latent class analysis with adult females, [ 29 ] found that one pathway to adult BPD emanated from a childhood profile with at least low/moderate levels of hyperactive/impulsive symptoms but low levels of inattentive symptoms.
Finally, considered either categorically or dimensionally, ADHD is clearly linked with increased risk for self-harm (a common feature of BPD), including suicidal behavior and nonsuicidal self-injury (NSSI) (see [ 30 ] for a recent review). Notably, females with ADHD, especially those with high levels of impulsivity as characterized by the ADHD-C presentation, are markedly at risk for attempted suicide and moderate-to-severe NSSI [ 31 ]. Mechanisms linking ADHD with later self-harm include internalizing and externalizing symptoms, as well as peer victimization and peer rejection [ 30 ]. Risk for suicidality is greatly increased when females with ADHD have histories of childhood maltreatment [ 32 ].
Executive functioning (EF)
EF includes goal-oriented cognitive processes such as planning, inhibition, organization, set shifting, working memory, and problem solving. EF deficits have frequently been linked to both ADHD and BPD. For a review of ADHD and EF see Brown [ 33 ]; for a review of BPD and EF, see Garcia-Villamisar et al. [ 34 ]. In general, individuals with BPD show greater EF deficits than typically developing controls [ 35 ]. Individuals with BPD have demonstrated EF deficits in the domains of planning [ 36 , 37 ], working memory [ 38 ], response inhibition and problem solving [ 39 ], and motor inhibition [ 40 ]. Additionally, a meta-analysis revealed that BPD samples with higher rates of comorbid psychopathology performed worse on EF tasks compared to samples with lower rates of comorbidity [ 41 ]. However, few prospective longitudinal studies have examined childhood EF as predictive of later BPD, with the notable exception of Belsky et al. [ 26 ], who found that a composite measure of EF deficits at age 5 was related to BPD symptoms at age 12. Longitudinal investigation of global measures of EF and relations to BPD are critically needed.
Early internalizing and externalizing symptoms
BPD is commonly comorbid with a variety of other psychological disorders, both internalizing and externalizing in nature [ 42 ]. In a systematic review of risk factors for BPD from longitudinal research, Stepp et al. [ 43 ] found that 16 of 19 studies examining internalizing and externalizing psychopathology yielded predictions to later BPD [ 9 ]. That is, dimensions of internalizing (depression) and externalizing (substance use disorder) behaviors in adolescence were associated with subsequent adult BPD symptoms. Indeed, existing literature theorizes that adolescence is a sensitive period for the development of personality disorders—and that personality disorders are preceded by internalizing and externalizing symptoms, not the other way around [ 44 ]. Additionally, some evidence indicates that internalizing and externalizing symptoms in childhood are also related to later BPD symptoms (Belsky et al., [ 26 ]; Geselowitz et al., [ 10 ] but see Burke [ 23 ] & Stepp, [ 18 ], for negative results). Hypothesized mechanisms include emotion dysregulation, which characterizes both internalizing and externalizing psychopathology [ 11 ]. In short, greater understanding of the contribution and developmental timing of internalizing and externalizing symptoms has the potential to inform early interventions to prevent the development of clinically significant BPD symptoms.
Adverse childhood experiences/trauma
Consistent with Linehan’s Biosocial Model, a large body of research has linked a history of environmental invalidation and adversity—and at its extreme, trauma—to the development of BPD [ 1 ]. A history of physical abuse, sexual abuse, and neglect in childhood has long been linked with BPD [ 9 ]. For key prospective longitudinal investigations, see Johnson et al. [ 45 ] and Widom et al. [ 46 ]. Having a parent with psychopathology (including depression and substance use problems) has consistently been found to be a family-related risk factor for BPD [ 9 , 43 ]. Empirical research on the role of parenting and parent–child transactions has been limited [ 47 ], even though key theories posit that transactions between a child’s biological sensitivity and adverse environments (including family factors and parenting) both lead to and maintain BPD symptomology [ 1 ] as well self-harmful behaviors in early adulthood [ 48 ]. High levels of parental depression and parental stress have been linked to BPD [ 49 ], as well as escalation of negative affect and behaviors in mother-daughter conflict situations [ 47 ]. In a prospective, longitudinal study of twins followed from age 5 to 12, children who were physically maltreated or exposed to high maternal negative expressed emotion developed high levels of BPD characteristics [ 26 ], replicating other prospective studies [ 25 , 50 , 51 ]. Still, at least one study revealed that maternal parenting stress in adolescence was not related to adolescent BPD symptom severity [ 52 ]. More research is needed related to transactions between parents and their offspring in terms of the development of BPD [ 53 ].
Present study and hypotheses
In sum, numerous risk factors for BPD have been posited, including ADHD symptom dimensions, low executive functioning, early internalizing and externalizing psychopathology, and childhood adversity and trauma. Yet with the clear exception of Beeney et al. [ 8 ], little research has examined such factors simultaneously, limiting current understanding of the independent or combined contributions of such variables. Also, many studies examine delimited developmental periods (e.g., childhood to adolescence, adolescence to young adulthood). Finally, there is a dearth of research examining the core ADHD dimensions of hyperactivity/impulsivity and inattention as related to risk for later BPD (for a review, see Beauchaine et al. [ 11 ]).
We leverage a sample of females with childhood-diagnosed ADHD and a matched comparison sample followed prospectively from childhood through young adulthood. Consistent with Linehan’s Biosocial Model, recent developmental models of females with ADHD [ 11 ], and extant literature, we hypothesize that both childhood and adolescent (a) hyperactivity/impulsivity and (b) adversity/trauma will emerge as significant risk factors for BPD after adjusting for demographic covariates as well as additional evidence-based risk factors. We also predict that, by late adolescence, internalizing and externalizing symptoms will be significant predictors of young adult BPD. An exploratory aim is to examine if childhood socioeconomic status (SES) moderates associations between predictors of interest and later BPD. We aim to add to the literature on developmental risk factors for BPD to inform existing models of BPD development and prevention approaches.
Procedure and participants
The current data were drawn from an ongoing prospective, longitudinal study of females with and without carefully diagnosed childhood ADHD (see Hinshaw, [ 54 ] for more complete details). This study was approved by the Committee for the Protection of Human Subjects (CPHS) at the University of California, Berkeley. Participants were initially recruited across a metropolitan area from schools, mental health centers, pediatric practices, and through advertisements to participate in research-based, 5-week summer day camps between 1997–1999. Some participants were recruited through the general population whereas others were recruited through the healthcare system. These programs were designed to be enrichment programs featuring classroom and outdoor environments for ecologically valid assessment, rather than intensive therapeutic interventions. All participants and their families underwent a rigorous, multi-step psychodiagnostic assessment process (see below), after which 140 girls with ADHD and 88 age- and ethnicity-matched comparison girls were selected to participate in the childhood program (Wave 1; M age = 9.6 years, range = 6–12 years).
Following recruitment, all participants were screened for ADHD regardless of if they had already had a pre-established diagnosis. To establish a baseline diagnosis of ADHD, we used the parent-administered Diagnostic Interview Schedule for Children, 4 th ed. (DISC-IV) [ 55 ] and SNAP rating scale [ 52 ], Hinshaw, [ 54 ] for the diagnostic algorithm). Comparison girls could not meet diagnostic criteria for ADHD on either measure. Some comparison girls met criteria for internalizing disorders (3.4%) or disruptive behavior disorders (6.8%) at baseline, yet our goal was not to match ADHD participants on comorbid conditions but instead to obtain a representative comparison group. Exclusion criteria included intellectual disability, pervasive developmental disorders, psychosis, overt neurological disorder, lack of English spoken at home, and medical problems preventing summer camp participation. The final sample included 228 girls with ADHD-Combined presentation ( n = 93) and ADHD-Inattentive presentation ( n = 47), plus an age- and ethnicity-matched comparison sample ( n = 88). Participants were ethnically diverse (53% White, 27% African American, 11% Latina, 9% Asian American), reflecting the composition of the San Francisco Bay Area in the 1990’s. Family income was slightly higher than the median local household income in the mid-1990s, yet income and educational attainment of families were highly variable, ranging from professional families to those receiving public assistance. On average, parents reported being married and living together (65.8%) at the baseline assessment.
Participants were then assessed 5 (Wave 2; M age = 14.2 years, range = 11–18; 92% retention [data not included from this wave in the present study]), 10 (Wave 3; M age = 19.6 years, range = 17–24 years; 95% retention), and 16 (Wave 4; M age = 25.6 years, range = 21–29 years; 93% retention) years later. Data collection included multi-domain, multi-informant assessments, performed in our clinic for most individuals; when necessary, we performed telephone interviews or home visits. We obtained informed consent from all participants (for initial waves: all legal guardians for minors (if age was below 18 years) and parents; for later waves: all participants and parents). Participants received monetary compensation. For additional information see Hinshaw et al. [ 31 , 56 ], Owens et al. [ 57 ].
Predictor variables
Predictor variables were measured during the baseline assessment at Wave 1 (childhood), with repeated assessment of several key measures at Wave 3 (late adolescence), to incorporate risk factors in both developmental periods.
ADHD Symptom Severity: Swanson, Nolan, and Pelham rating scale, 4 th Ed. (SNAP-IV; Swanson, [ 58 ] ). We measured severity of both hyperactivity/impulsivity (SNAP-HI) and inattentive (SNAP-IA) symptoms using an average of parent- and teacher-report (childhood) or parent- and self-report (late adolescence) on a dimensionalized checklist of these two respective symptom domains (9 items for each) to obtain multi-informant composite scores (SNAP-HI: α = 0.950; SNAP-IA: α = 0.968). For example, items included “…this child is forgetful in daily activities” and “…this child blurts out answers to questions before the questions have been completed.” The severity of each symptom was scored 0 (not at all) to 3 (very much). Thus, scores of both hyperactivity/impulsivity and inattention symptoms ranged from 0–27, with higher scores indicating more severe symptomology. The SNAP-IV is a widely used scale of ADHD symptom severity in both research and clinical settings (e.g., MTA Cooperative Group, [ 59 ]). It has good internal consistency and test–retest reliability [ 60 ].
Executive Functioning: Rey Osterrieth Complex Figure (ROCF) [ 61 ]. We measured executive functioning using the ROCF, a laboratory-based cognitive task requesting that an individual copy and later recall a complex image composed of 64 segments. The ROCF measures multiple domains of executive functioning such as planning, inhibitory control, attention to detail, working memory, and organization. It is often considered a more “global” measure of executive functioning [ 62 ]. We analyzed the Copy condition of this task, during which participants are timed as they view the stimulus figure and draw the figure on a blank piece of paper. For scoring, we used the Error Proportion Score (EPS; the ratio of number of errors divided by the total number of segments drawn), a well-validated method of scoring the ROCF, indexing efficiency [ 63 ]. In previous research with this sample, only the Copy condition (versus Delayed Recall condition) differentiated girls with ADHD from our comparison sample at baseline. The ROCF EPS showed the largest effect size ( d = 0.90) out of all other EF measures in our battery (Hinshaw et al., [ 64 ]; Sami et al., [ 63 ]). As well, childhood EPS predicts later academic and occupational functioning in comparison to other EF measures Miller et al., [ 62 ]).
Internalizing and Externalizing Symptoms: Child Behavior Checklist, Adult Self Report, and Adult Behavior Checklist (CBCL; ASR; ABCL) [ 65 , 66 ] . In childhood, we measured severity of internalizing (α = 0.89) and externalizing (α = 0.93) symptoms via parent-report on the Internalizing and Externalizing scales of the CBCL. In late adolescence, we averaged participant self-report on the Adult Self-Report (ASR) and parent-report on the Adult Behavior Checklist (ABCL) to obtain multi-informant composite scores. The ASR and ABCL are parallel versions of the CBCL for older individuals. We used T -scores ( M = 50, SD = 10) as dimensional symptom measures, with scores above 60 indicating elevated/at-risk and scores above 70 indicating clinically significant symptoms. For example, items included: “…. your child feels worthless or inferior” (internalizing) “…your child gets in many fights” (externalizing). The CBCL, ASR, and ABCL have good–excellent validity, test–retest reliability, and internal consistency [ 66 , 67 ].
Parent Psychopathology: Beck Depression Inventory (BDI-I; BDI-II) [ 68 , 69 ] . We measured depressive symptoms of the primary caregiver (typically the mother) using self-report on the BDI-I at Wave 1 and the BDI-II at Wave 3. Mothers rated each of the 21 items on a 4-point severity scale. For example, items included a choice between “1.) I do not feel sad. 2.) I feel sad. 3.) I am sad all the time and I can’t snap out of it. 4.) I am so sad or unhappy I can’t stand it.” Total possible scores could range from 0–63, with higher scores indicating greater severity of depression. The BDI is a widely used and extensively validated self-report measure of depression in adults [ 70 ].
Parenting Stress Due To Dysfunctional Interactions: Parenting Stress Index-Short Form (PSI-SF) [ 71 ] . We measured stress-inducing dysfunctional parent–child interactions using the PSI-SF, a widely used self-report measure assessing stress experienced by parents related to their role as a parent. In particular, we used the 12-item Parental-Child Dysfunctional Interaction (PCDI) subscale which measures a parent’s perception of dysfunction in the parent–child relationship that contributes to the parent’s feelings of parental stress. Participants’ mothers rated each item on a scale from 1 (strongly agree) to 5 (strongly disagree). For example, items included: “My child does not like me or want to be close.” Higher scores indicated higher levels of maternal parenting stress. The PSI-SF has demonstrated good test-test reliability, internal consistency, and validity, with the reliability of the subscales ranging from 0.68 to 0.85 and the internal consistency ranging from 0.80 to 0.87 [ 72 , 73 ]. In our sample, the internal consistency (Cronbach’s alpha) of the Parental-Child Dysfunctional Interaction subscale at Wave 1 and Wave 3 were 0.88 and 0.93 respectively.
Cumulative childhood adversity: Adverse Childhood Experiences questionnaire (ACE) [ 74 ] . We measured cumulative experiences of childhood adversity via retrospective report by on the ACE questionnaire at Wave 4, which assesses experiences of childhood abuse, neglect, and household dysfunction during the first 18 years of life. ACE scores ranged from 0–10, with higher scores indicating experiences of multiple types of childhood adversity. For example, items included: “Did you often or very often feel that no one in your family loved you or thought you were important or special?” The ACE questionnaire is a commonly used measure to assess for the cumulative effect of multiple forms of childhood adversity [ 75 ], and has good reliability and validity [ 76 ]—including at least moderate test–retest reliability of retrospective reports [ 77 ].
Criterion variables
These were measured at Wave 4 (Young Adulthood).
Borderline Personality Disorder Diagnosis. A licensed clinical psychologist or a graduate student in clinical psychology, under close supervision, conducted a clinical interview with participants using the Structured Clinical Interview for DSM-IV-TR (SCID) [ 78 ] and the Borderline Personality Disorder (BPD) module of the SCID-II (SCID-II) [ 79 ]. The SCID-II is a semi-structured interview widely used in both research and clinical practice, with research indicating good to excellent inter-rater reliability [ 80 ]. A participant met criteria for a diagnosis of BPD if the clinician rated the participant at or above threshold on five of the nine symptom traits. A single dichotomous variable (0 or 1) reflected a BPD diagnosis.
Borderline Personality Disorder Dimensional Features. Because both diagnostic interview and self-report measures may yield optimal assessment of BPD [ 81 ], we also included a dimensional measure of BPD in order to assess and validate the categorical measure of BPD. For a large subset of the sample, a 15-item self-report scale was included, based on the BPD module of the Structured Clinical Interview for DSM-5 Axis II disorders (SCID-II) [ 82 ]. However, every participant did not complete this self-report measure, as it was added after data collection began. Additionally, some participants completed only interviews and did not return their packet of questionnaires including this measure. Each item of the measure is rated dichotomously (0 = No, 1 = Yes), so that the total possible score ranged from 0–15, with higher scores indicating more features of BPD. For example, items included: “Have you often become frantic when you thought that someone you really cared about was going to leave you?” This scale is consistent with DSM-5 BPD criteria, and has been used in several other studies, with satisfactory internal reliability (α = 0.81) [ 83 , 84 ].
To ascertain whether domains of impairment were related specifically to BPD status, we added covariates empirically associated with BPD and associated predictors: (1) SES—a composite measure of parent report of family income and maternal education in childhood; (2) parent report of child’s race/ethnicity in childhood; and (3) participant age in young adulthood.
Data analytic plan
Statistical analyses were performed with RStudio, version 1.2.1335. First, we computed descriptive statistics and zero-order correlations across potential predictors, background variables of interest, and young adult BPD (measured both categorically and dimensionally). Second, we conducted a series of (a) binary logistic regressions to test whether each theory-informed predictor independently predicted a young-adult diagnosis of BPD and (b) parallel linear regressions regarding dimensional features of BPD. We calculated effect sizes of Cohen’s d for the dichotomous criterion and R 2 for the dimensional measure. Given the many initial predictors, we deployed the stringent criterion that a predictor be retained for subsequent analyses only if it displayed a medium (or larger) effect size in relation to the respective categorical or dimensional measure of BPD. For Cohen’s d, we considered effect sizes ≧ 0.2 as small, ≧ 0.5 as medium, and ≧ 0.8 as large; for R 2 , we considered ≧ 0.02 as small, ≧ 0.13 as medium, and ≧ 0.26 as large (Cohen, 1988). Third, we tested whether predictors meeting this criterion continued to do so when adjusting for sociodemographic covariates (baseline SES, participant race/ethnicity, and participant age), using (a) binary logistic regressions or (b) linear regressions, respectively.
We added predictors maintaining significance into separate models by developmental period (Model 1 = childhood; Model 2 = late adolescence), Given the small subset with a BPD diagnosis, we used Firth’s penalized likelihood method in binary logistic regressions to minimize bias introduced by several independent variables [ 85 ]. For exploratory moderator analyses, we conceptualized a moderator as a baseline factor that might reveal differential predictor-criterion associations at different levels of the putative moderator [ 86 ]. Our moderator of interest included baseline (Wave 1) socioeconomic status. Understanding that such analyses are non-hypothesis-driven, we placed interaction terms of the putative predictor x SES moderator at the third step of each significant predictor regression model.
Descriptive analyses and correlations
A total of 19 participants met criteria for a diagnosis of BPD. Fourteen (74%) had received a childhood diagnosis of ADHD (χ 2 (3, N = 199) = 1.1, p = 0.3, OR : 1.31, CI: 0.79, 2.17), with a majority of them having received a childhood diagnosis of ADHD-C (58%).
Tables 1 , 2 , 3 and 4 present intercorrelations among key variables. Because maternal- and teacher-report of childhood hyperactivity/impulsivity (W1 SNAP-HI), inattention (W1 SNAP-IA), overt aggression (W1 CSBS), and relational aggression (W1 CSBS), plus maternal- and self-report of late adolescent hyperactivity/impulsivity (W3 SNAP-HI), inattention (W3 SNAP-IA), externalizing symptoms (W3 ASR/ABCL), and internalizing symptoms (W3 ASR/ABCL) were highly correlated, we averaged ratings across mother and teacher (childhood) and mother and self (early adulthood) to create a composite score for each domain.
For young-adult categorical BPD diagnoses, significant childhood point biserial correlates included hyperactivity/impulsivity (W1 SNAP-HI; r pb = 0.17, p < 0.05), low executive functioning (W1 ROCF; r pb = 0.22, p < 0.01), and a history of overall adversity (W4 ACEs; r pb = 0.32, p < 0.01) (see Table 1 ). Significant late-adolescent point biserial correlates included hyperactivity/impulsivity (W3 SNAP-HI; r pb = 0.40, p < 0.01), inattention (W3 SNAP-IA; r pb = 0.38, p < 0.01), externalizing symptoms (W3 ASR/ABCL; r pb = 0.39, p < 0.01), internalizing symptoms (W3 ASR/ABCL ; r pb = 0.34, p < 0.01), and maternal psychopathology (W3 BDI-II ( r pb = 0.16, p < 0.05) (see Table 2 ).
Regarding young-adult dimensionally scored features of BPD, childhood hyperactivity/impulsivity (W1 SNAP-HI; r = 0.43, p < 0.01), childhood inattention (W1 SNAP-IA; r = 0.29, p < 0.01), low executive functioning (W1 ROCF; r = 0.25, p < 0.01), externalizing symptoms (W1 CBCL; r = 0.36, p < 0.01), internalizing symptoms (W1 CBCL; r = 0.24, p < 0.01), overt aggression (W1 CSBS; r = 0.38, p < 0.01), relational aggression (W1 CSBS; r = 0.32, p < 0.01), negative peer nominations (W1 Peer Report; r = 0.35, p < 0.01), and a cumulative history of childhood adversity (W4 ACEs; r = 0.47, p < 0.01) were significant correlates. Late adolescent hyperactivity/impulsivity (W3 SNAP-HI; r = 0.52, p < 0.01), inattention (W3 SNAP-IA; r = 0.43, p < 0.01), low executive functioning (W3 ROCF;; r = 0.20, p < 0.05), externalizing symptoms (W3 ASR/ABCL; r = 0.63, p < 0.01), internalizing symptoms (W3 ASR/ABCL ; r = 0.57, p < 0.01), maternal psychopathology (W3 BDI-II; r = 0.25, p < 0.01), and maternal parenting stress due to dysfunctional interactions (W3 PSI-PCDI; r = 0.23, p < 0.05) were all significantly correlated with young adult BPD features (Table 4 ).
Predictors of young adult BPD diagnosis
In the binary logistic regressions with Firth’s penalized likelihood method, conducted to assess independent predictors of the dichotomous outcome of meeting (vs. not meeting) diagnostic criteria for BPD in young adulthood, we initially tested whether each predictor of interest was significantly associated with BPD, followed by inclusion of (a) covariates and (b) other significant predictor variables according to developmental period (Table 5 ).
Among childhood predictors, hyperactivity/impulsivity ( p < 0.05; d = 0.58) and low executive functioning ( p < 0.01; d = 0.76) each predicted BPD diagnostic status in young adulthood, but only low executive functioning maintained significance after adjusting for covariates ( p < 0.05). As well, the childhood ACE score was a significant predictor, even with adjustment for covariates ( p < 0.001; d = 1.14). Regarding for late-adolescent predictors, hyperactivity/impulsivity ( p < 0.001; d = 1.45), inattention ( p < 0.001; d = 1.36), externalizing ( p < 0.001; d = 1.41), and internalizing ( p < 0.001; d = 1.23) symptoms each predicted young adult BPD, adjusting for covariates. Maternal psychopathology did not survive inclusion of covariates ( p = 0.093).
Finally, we entered all predictors with a medium or larger effect size (Cohen’s d ≧ 0.5) that had maintained significance after inclusion of covariates into models divided by developmental period. In childhood, low executive functioning ( p = 0.012) and the ACE score maintained significance ( p = 0.003). In the late-adolescent predictor model, only inattentive symptoms maintained marginal significance ( p = 0.059), but hyperactivity/impulsivity ( p > 0.05), internalizing symptoms ( p > 0.05), and externalizing symptoms ( p > 0.05) did not.
Predictors: Young adult dimensional BPD features
Via linear regressions, childhood hyperactivity/impulsivity ( p < 0.001; R 2 = 0.182), inattention ( p < 0.001; R 2 = 0.079), low executive functioning ( p = 0.004; R 2 = 0.054), externalizing symptoms ( p < 0.001; R 2 = 0.121), internalizing symptoms ( p = 0.004; R 2 = 0.051), overt aggression ( p < 0.001; R 2 = 0.137), relational aggression ( p < 0.001; R 2 = 0.094), negative peer nominations ( p < 0.001; R 2 = 0.114), and maternal psychopathology ( p = 0.045; R 2 = 0.020) independently predicted young-adult features of BPD. Of these, only childhood hyperactivity/impulsivity ( p < 0.001), inattention ( p < 0.001), externalizing symptoms ( p < 0.001), internalizing symptoms ( p < 0.05), overt aggression ( p < 0.001), relational aggression ( p < 0.001), and negative peer nominations ( p < 0.001) maintained significance after adjusting for covariates. Maternal parenting stress due to dysfunctional interactions became significant after adjusting for covariates ( p < 0.05). The ACE score significantly predicted young adult BPD features ( p < 0.001; R 2 = 0.213), even after adjusting for covariates ( p < 0.001).
For late-adolescent predictors, hyperactivity/impulsivity ( p < 0.001; R 2 = 0.265), inattention ( p < 0.001; R 2 = 0.177), low executive functioning ( p < 0.05; R 2 = 0.033), externalizing symptoms ( p < 0.001; R 2 = 0.398), internalizing symptoms ( p < 0.001; R 2 = 0.317), maternal psychopathology ( p < 0.01; R 2 = 0.053), and maternal parenting stress due to dysfunctional interactions ( p < 0.05; R 2 = 0.043) each independently predicted features of BPD in young adulthood. Of these, hyperactivity/impulsivity ( p < 0.001), inattention ( p < 0.001), externalizing symptoms ( p < 0.001), internalizing symptoms ( p < 0.001), maternal psychopathology ( p < 0.05), and maternal parenting stress due to dysfunctional interactions ( p < 0.01) maintained significance after adjusting for covariates. Low executive functioning did not.
Finally, we entered predictors with a medium (or above) effect size ( R 2 ≧ 0.13)—that had maintained significance after inclusion of covariates—into separate models by developmental period. In childhood, only childhood hyperactivity/impulsivity ( p < 0.01) and the ACE score maintained significance ( p < 0.001), but overt aggression did not ( p > 0.05). As for late-adolescent predictors, only externalizing ( p < 0.001) and internalizing symptoms ( p < 0.01) maintained significance—but not hyperactivity/impulsivity ( p > 0.05) or inattention ( p > 0.05).
Exploratory moderator analyses
Regarding categorical young adult BPD diagnosis, no predictor x moderator interactions emerged as statistically significant. For young adult dimensional BPD features, only an interaction between (a) low childhood executive functioning (predictor) and (b) low childhood socioeconomic status (moderator) (W1 SES; Δ R 2 = 0.022, p < 0.05) emerged as statistically significant. Here, it was the combination of low executive functioning and low baseline SES that predicted higher levels of BPD dimensional features.
Leveraging a well-characterized longitudinal female sample with and without carefully diagnosed childhood ADHD, we examined theory-informed predictors of young adult BPD—considered both categorically and dimensionally—from childhood and late-adolescent timespans. Although we emphasize caution regarding interpretation of findings due to our small sample size, this investigation extends research from our laboratory on developmental predictors of self-harm behaviors [ 87 ] to include borderline personality disorder as a criterion measure. We note that individuals with BPD—a condition characterized by intense and pervasive dysregulation of emotion, behavior, cognition, and relationships—may or may not engage in self-harm.
First, regarding our categorical measure of BPD, using binary logistic regressions with correction for small sample size, we found that—as hypothesized—a cumulative history of childhood adversity, as measured by the ACE score, predicted BPD diagnosis. Low EF in childhood was also a significant predictor, even after adjusting for ACE scores and demographic covariates. Regarding late-adolescent predictors, hyperactivity/impulsivity, inattention, internalizing, and externalizing symptoms each independently predicted young adult BPD diagnosis after adjusting for covariates, but maternal depression did not. In stringent analyses accounting for all independently significant late adolescent predictors, only symptoms of inattention were independently (albeit marginally) related to young adult BPD diagnosis.
Second, with respect to our dimensional measure of BPD features, we found—consistent with hypotheses—that both childhood hyperactivity/impulsivity and a cumulative history of childhood adversity from the ACE score predicted young adult BPD features, with adjustment for covariates. Furthermore, childhood inattention, externalizing symptoms, internalizing symptoms, overt aggression, relational aggression, negative peer nominations, and maternal parenting stress due to dysfunctional interactions also independently predicted young adult BPD features after adjusting for covariates. Yet in the final model, including all childhood predictors with a medium (or larger) effect size that had survived covariates, only childhood hyperactivity/impulsivity and the ACE score maintained significance. As for late-adolescent predictors of the dimensional outcome, hyperactivity/impulsivity, inattention, externalizing symptoms, internalizing symptoms, maternal psychopathology, and maternal parenting stress due to dysfunctional interactions maintained significance after adjusting for covariates, but low executive functioning did not. In the final analysis, adding all surviving predictors in the same model, only late-adolescent externalizing and internalizing symptoms maintained significance. Finally, as for exploratory moderator analyses, we found an interaction between low childhood executive functioning and low socioeconomic status at baseline was significant, suggesting that socioeconomic disadvantage may compound the predictive effects of low executive functioning with respect to later BPD dimensional scores.
Overall, the child and adolescent predictors of later BPD are largely consistent with those from previous investigations [ 8 , 10 , 18 , 25 , 26 , 43 ], emerging here from a carefully controlled prospective investigation. Regarding ADHD symptoms, almost 75% of women who met criteria for BPD in young adulthood had diagnoses of childhood ADHD, most often characterized by high levels of impulsivity (ADHD-C). This finding is consistent with both cross-sectional and longitudinal research, as well as theoretical models of the developmental course of individuals with high levels of early impulsivity, related to BPD as an end-point [ 11 ].
For ADHD dimensions, our findings add to the limited number of studies examining hyperactive, impulsive, and inattentive symptoms and their severity across development, especially beginning in childhood [ 8 , 25 , 26 , 27 ]. That hyperactivity/impulsivity in childhood and adolescence did not significantly predict later categorical BPD diagnosis was unexpected and may relate to our small sample size. Yet regarding our dimensional measure, when adjusting for covariates and other predictors, hyperactivity/impulsivity in childhood did significantly predict later BPD features. This finding is consistent with the only two other known studies to our knowledge that have examined prospective associations between childhood impulsivity and later BPD [ 26 , 27 ]. Two studies have found prospective prediction from both adolescent hyperactivity/impulsivity and inattention to later BPD [ 8 , 25 ]—along this line, note our marginally significant prediction of categorical BPD from late-adolescent inattentive symptoms: In both Carlson et al. [ 25 ] and a recent machine learning study of 128 variables related to risk for BPD, inattention in adolescence emerged as an important predictor [ 8 ]. Each dimension of ADHD appears to play an important role in the development of BPD symptoms.
The finding linking low EF in childhood to young adult BPD diagnosis is also consistent with previous (yet limited) research. In the only known prospective longitudinal study to date examining childhood EF as predictive of later BPD, a composite measure of EF at age 5 predicted BPD symptoms at age 12 [ 26 ]. When we examined low childhood EF and BPD dimensional features, our findings were not significant. Still, moderator analyses revealed that girls with both low EF and low socioeconomic status were at especially risk for high levels of BPD features. Perhaps difficulties in low EF are related to high or clinically significant BPD in the context of socioeconomic disadvantage.
Regarding internalizing and externalizing symptoms, we found that high levels of each were related to later BPD features after adjusting for other important predictors—but not when we measured BPD categorically. Furthermore, multiple forms of aggression in childhood including both overt and relational aggression, plus negative peer nominations, predicted young adult BPD features, but these findings did not maintain significance in the presence of other important predictors. Thus, symptoms of aggression and peer preference are important in childhood as risk factors for later BPD, yet other factors—childhood hyperactivity/impulsivity and trauma-remain statistically superior. Indeed, there was substantial overlap in our measures of aggression, negative peer nomination, hyperactivity/impulsivity, and broadband externalizing symptoms. Overall, our key findings replicate those from Stepp et al. [ 43 ], who showed that adolescent internalizing and externalizing symptoms predict adult BPD (for additional research, see Belsky et al., [ 26 ]; and Geselowitz et al., [ 10 ]). Adolescence appears to be a particularly sensitive period during which vulnerability for the development of severe and pervasive dysregulation across the lifespan may be realized [ 44 ].
Although maternal psychopathology—plus both child and late-adolescent maternal parenting stress due to dysfunctional interactions—were each independently associated with young adult BPD features after adjusting for covariates, their effect sizes were small. Any implications require replication. Findings from other research indicate that parental invalidation and negative parenting practices may well be stronger predictors [ 53 ].
Consistent with a large body of research linking a history of childhood adversity/trauma with later BPD [ 88 ], we found that a cumulative history of childhood adversity, measured by the ACE scale, was a crucial predictor of both young-adult BPD diagnosis and dimensional features. This measure of cumulative history of childhood adversity is retrospective—and may therefore be better characterized as a subjective experience of childhood trauma rather than objective experiences of childhood trauma. These findings are consistent recent data finding that risk of psychopathology is high among individuals with subjective reports of childhood maltreatment regardless of whether these experiences were validated by objective measures [ 89 ]. As well, the ACE measure we used constitutes the gold standard in the field.
Our results support theories that transactions between dispositional and environmental factors over time can lead to a cycle of dysregulation of emotion, behavior, and cognition as well as difficult interpersonal relationships [ 1 , 11 ]. Indeed, findings support Linehan’s Biosocial Theory plus recent developmental models of females with ADHD [ 11 ]. That is, behaviorally expressed impulsivity may be a risk factor for a range of outcomes, including BPD. As development progresses, children with trait impulsivity may experience childhood trauma—linked with, for example, intergenerational trauma, maladaptive parenting practices (especially in relation to the child’s impulsive behavior), and/or parents’ own behavioral impulsivity—which may then transactionally escalate the development of BPD. The original impulsivity may, via heterotypic continuity, come to be expressed as a combination of internalizing and externalizing dimensions, leading to BPD [ 11 , 90 ]—a suggestion requiring further empirical investigation. Future research should include prospective temporal assessment of these domains, as well as other environmental mediators (e.g., peer relationship influences, substance use) and valid measures of behavioral parental invalidation, to assess multi-factor etiological influences.
Clinical implications
Although our sample size is too small to draw definitive clinical recommendations, we provide several ideas for possible clinical and public health implications, emphasizing caution in interpretation of results related to study limitations (see below for more detail in this regard). First, findings highlight the longstanding effects of early experiences of adversity and trauma. Prevention of these childhood experiences, especially through public health initiatives, cannot be overemphasized. Second, our results reveal the importance including global EF deficits in childhood as indicators of risk for BPD, in addition to the focus on childhood impulsivity. These findings have implications for guiding early clinical assessment and intervention (e.g., through early EF skills training) to prevent later BPD. In short, we highlight the need for interventions before the adolescent period, which appears to be an especially sensitive time of risk [ 11 ].
Children with histories of adversity/trauma and/or deficits in EF could receive interventions targeting emotion dysregulation, a mechanism linked to the development of BPD, such as Dialectical Behavior Therapy for Children (DBT-C) [ 91 ], Parent–Child Interaction Therapy (PCIT) [ 92 ], or creative combinations of these therapies [ 93 ]. Widespread assessment of early risk factors to identify individuals at risk remains a challenge. We also recommend that evidence-based treatments for severe emotion dysregulation (i.e., DBT) include remediation of EF deficits.
Limitations and future directions
Our study has several important limitations. First, our sample size is small for the categorical BPD variable, with only 19 females meeting diagnostic criteria for BPD in young adulthood, clearly limiting statistical power. Note that we used Firth’s penalized likelihood method to statistically account for our small sample [ 94 ]. Furthermore, only a subset of our sample completed the self-report dimensional BPD measure. We emphasize the need for replication and cautious interpretation of findings. Second, we did not have symptom-level data available for our categorical measure of BPD, preventing us from evaluating clinician-assessed dimensions of BPD symptoms. Future research would benefit from examining dimensional severity of BPD symptoms, as well as specific traits, some of which have recently been linked to increased risk for a suicide attempt [ 95 ]. Third, several measures—including those of BPD features, cumulative trauma history, and ADHD (in part) were self-reported—and may thus be subject to bias. Fourth, we were not able to peform mediator analyses and therefore cannot add to the literature on potential “driving” mechanisms between childhood and adulthood (e.g., emotion dysregulation). Fifth, we did not separate predictor symptom domains of hyperactivity vs. impulsivity, as psychometrics are superior when using the full 9-item Hyperactivity/Impulsivity scale. As well, this measure is more consistent with the DSM’s layout of symptoms. Although we support the separation of theses symptoms in future research—see the excellent national analysis by Tiger et al. [ 27 ]—we elected to include the full 9-item scale. Sixth, our measure of externalizing symptoms in late adolescence (ASR, ABCL) included measures of aggression, but given our multiple testing, we did not examine aggression per se during this developmental window. Future research would benefit from examining aggressive symptoms across development, given empirical research and theory linking high levels aggression and peer problems with later BPD [ 11 , 18 ]. Seventh, there is controversy over whether the Rey-Osterrieth Complex Figure Test captures meaningful variance in executive functioning [ 96 ]. It could be that this measure is a better index of visual-motor integration and overall neuropsychological functioning than of executive functioning [ 97 , 98 ]. Future research should investigate different domains of neuropsychological functioning and BPD development. Eighth, there is definitional overlap between ADHD and BPD, given that both are characterized by impulsivity, which could account for some of the present results. Finally, a key limitation is the timing of our BPD measure—we measured BPD only during young adulthood, but some participants may already have met criteria for BPD in adolescence.
Still, key strengths include a carefully diagnosed, ethnically and socioeconomically diverse sample of females; emphasis on multi-domain and multi-informant measures; high sample retention; and a prospective (and ongoing) longitudinal design. Moreover, we included stringent use of covariates and statistical penalization. Finally, we examined multiple domains of risk for BPD simultaneously and included several measures of BPD symptomology.
The current findings add to existing research on developmental pathways to BPD, especially among females with ADHD. Future directions should include replication, further examination of dimensions of both ADHD and EF, and distinct types of traumatic life events across development [ 99 ] as related to later BPD. Sensitive measures of early emotional invalidation are also necessary [ 53 ].
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Adverse childhood experiences scale
Attention-deficit/hyperactivity disorder
Attention-deficit/hyperactivity disorder, combined presentation
Attention-deficit/hyperactivity disorder, inattentive presentation
Beck depression inventory
- Borderline personality disorder
Child behavior checklist
Children’s social behavior scale
Executive functioning
Hyperactivity/impulsivity
Inattention
Nonsuicidal self-injury
Parenting stress index
Parent–child dysfunctional interactions
Rey osterrieth complex figure task
Structured clinical interview for DSM disorders
Swanson, Nolan, and Pelham questionnaire
Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychol Bull. 2009;135(3):495–510.
Article PubMed PubMed Central Google Scholar
Pompili M, Girardi P, Ruberto A, Tatarelli R. Suicide in borderline personality disorder: a meta-analysis. Nord J Psychiatry. 2005;59(5):319–24.
Article PubMed Google Scholar
Olfson M, Blanco C, Marcus SC. Treatment of adult depression in the United States. JAMA Intern Med. 2016;176(10):1482–91.
Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry. 2001;58(6):590–6.
Article CAS PubMed Google Scholar
Comtois KA, Carmel A. Borderline personality disorder and high utilization of inpatient psychiatric hospitalization: Concordance between research and clinical fiagnosis. J Behav Health Serv Res. 2016;43(2):272–80.
Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiat. 2015;72(5):475–82.
Article Google Scholar
Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; 1993.
Beeney JE, Forbes EE, Hipwell AE, Nance M, Mattia A, Lawless JM, et al. Determining the key childhood and adolescent risk factors for future BPD symptoms using regularized regression: comparison to depression and conduct disorder. J Child Psychol Psychiatry. 2021;62(2):223–31.
Stepp SD, Lazarus SA, Byrd AL. A systematic review of risk factors prospectively associated with borderline personality disorder: Taking stock and moving forward. Personal Disord. 2016;7(4):316–23.
Geselowitz B, Whalen DJ, Tillman R, Barch DM, Luby JL, Vogel A. Preschool age predictors of adolescent borderline personality symptoms. J Am Acad Child Adolesc Psychiatry. 2021;60(5):612–22.
Beauchaine TP, Hinshaw SP, Bridge JA. Nonsuicidal self-injury and suicidal behaviors in girls: The case for targeted prevention in preadolescence. Clin Psychol Sci. 2019;7(4):643–67.
Matthies SD, Philipsen A. Common ground in Attention Deficit Hyperactivity Disorder (ADHD) and Borderline Personality Disorder (BPD)-review of recent findings. Borderline Personal Disord Emot Dysregul. 2014;1(3):1–13.
Google Scholar
Miller TW, Nigg JT, Faraone SV. Axis I and II comorbidity in adults with ADHD. J Abnorm Psychol. 2007;116(3):519–28.
Bernardi S, Faraone SV, Cortese S, Kerridge BT, Pallanti S, Wang S, et al. The lifetime impact of attention-deficit hyperactivity disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2012;42(4):875–87.
Andrulonis PA. Disruptive behavior disorders in boys and the borderline personality disorder in men. Ann Clin Psychiatry. 1991;3(1):23–6.
Philipsen A, Limberger MF, Lieb K, Feige B, Kleindienst N, Ebner-Priemer U, et al. Attention-deficit hyperactivity disorder as a potentially aggravating factor in borderline personality disorder. Br J Psychiatry. 2008;192:118–23.
Matthies S, Van Elst LT, Feige B, Fischer D, Scheel C, Krogmann E, et al. Severity of childhood attention-deficit hyperactivity disorder-a risk factor for personality disorders in adult life? J Pers Disord. 2010;25(1):101–14.
Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of Attention Deficit Hyperactivity Disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. J Abnorm Child Psychol. 2012;40(1):7–20.
Miller CJ, Flory JD, Miller R, Harty SC, Newcorn JH, Halperin JM. Childhood ADHD and the emergence of personality disorders in adolescence: A pospective follow-up study. J Clin Psychiatry. 2008;69(9):1477–84.
Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. J Am Acad Child Adolesc Psychiatry. 2000;39(11):1424–31.
Rey JM, Morris-Yates A, Singh M, Andrews G, Stewart GW. Continuities between psychiatric disorders in adolescents and personality disorders in young adults. Am J Psychiatry. 1995;152(6):895–900.
Fischer M, Barkley RA, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. J Abnorm Child Psychol. 2002;30(5):463–75.
Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. J Abnorm Child Psychol. 2012;40(1):35–44.
Thatcher DL, Cornelius JR, Clark DB. Adolescent alcohol use disorders predict adult borderline personality. Addict Behav. 2005;30(9):1709–24.
Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Dev Psychopathol. 2009;21(4):1311–34.
Belsky DW, Caspi A, Arseneault L, Bleidorn W, Fonagy P, Goodman M, et al. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Dev Psychopathol. 2012;24(1):251–65.
Tiger A, Ohlis A, Bjureberg J, Lundström S, Lichtenstein P, Larsson H, et al. Childhood symptoms of attention-deficit/hyperactivity disorder and borderline personality disorder. Acta Psychiatr Scand. 2022;146(4):370–80.
Article CAS PubMed PubMed Central Google Scholar
Cumyn L, French L, Hechtman L. Comorbidity in adults with attention-deficit hyperactivity disorder. Can J Psychiatry. 2009;54(10):673–83.
van Dijk F, Lappenschaar M, Kan C, Verkes RJ, Buitelaar J. Lifespan attention deficit/hyperactivity disorder and borderline personality disorder symptoms in female patients: A latent class approach. Psychiatry Res. 2011;190(2–3):327–34.
Hinshaw SP, Nguyen PT, O’Grady SM, Rosenthal EA. Annual Research Review: Attention-deficit/hyperactivity disorder in girls and women: underrepresentation, longitudinal processes, and key directions. J Child Psychol Psychiatry. 2022;63(4):484–96.
Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. J Consult Clin Psychol. 2012;80(6):1041–51. https://doi.org/10.1037/a0029451 .
Meza JI, Owens EB, Hinshaw SP. Response inhibition, peer preference and victimization, and self-harm: Longitudinal associations in young adult women with and without ADHD. J Abnorm Child Psychol. 2016;44(2):323–34.
Brown TE. A new understanding of ADHD in children and adults: Executive function impairments. New York, NY: Routledge; 2013.
Book Google Scholar
Garcia-Villamisar D, Dattilo J, Garcia-Martinez M. Executive functioning in people with personality disorders. Curr Opin Psychiatry. 2017;30(1):36–44.
Haaland V, Esperaas L, Landrø NI. Selective deficit in executive functioning among patients with borderline personality disorder. Psychol Med. 2009;39(10):1733–43.
Gvirts HZ, Harari H, Braw Y, Shefet D, Shamay-Tsoory SG, Levkovitz Y. Executive functioning among patients with borderline personality disorder (BPD) and their relatives. J Affect Disord. 2012;143(1–3):261–4.
Ruocco AC. The neuropsychology of borderline personality disorder: a meta-analysis and review. Psychiatry Res. 2005;137(3):191–202.
Hagenhoff M, Franzen N, Koppe G, Baer N, Scheibel N, Sammer G, et al. Executive functions in borderline personality disorder. Psychiatry Res. 2013;210(1):224–31.
Williams GE, Daros AR, Graves B, McMain SF, Links PS, Ruocco AC. Executive functions and social cognition in highly lethal self-injuring patients with borderline personality disorder. Personal Disord. 2015;6(2):107–16.
Lampe K, Konrad K, Kroener S, Fast K, Kunert HJ, Herpertz SC. Neuropsychological and behavioural disinhibition in adult ADHD compared to borderline personality disorder. Psychol Med. 2007;37(12):1717–29.
Unoka Z, Richman M J. Richman. Neuropsychological deficits in BPD patients and the moderator effects of co-occurring mental disorders: A meta-analysis. Clin Psychol Rev. 2016;44:1–12.
Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, et al. Borderline personality disorder co-morbidity: Relationship to the internalizing-externalizing structure of common mental disorders. Psychol Med. 2011;41(5):1041–50.
Stepp SD, Olino TM, Klein DN, Seeley JR, Lewinsohn PM. Unique influences of adolescent antecedents on adult borderline personality disorder features. Personal Disord. 2013;4(3):223–9.
Sharp C, Vanwoerden S, Wall K. Adolescence as a sensitive period for the development of personality disorder. Psychiatr Clin North Am. 2018;41(4):669–83.
Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Arch Gen Psychiatry. 1999;56(7):600–8.
Widom CS, Czaja SJ, Paris J. A prospective investigation of borderline personality disorder in abused and neglected children followed up into adulthood. J Pers Disord. 2009;23(5):433–46.
Whalen DJ, Scott LN, Jakubowski KP, McMakin DL, Hipwell AE, Silk JS, et al. Affective behavior during mother-daughter conflict and borderline personality disorder severity across adolescence. Personal Disord. 2014;5(1):88–96.
Gordon CT, Hinshaw SP. Parenting stress as a mediator between childhood ADHD and early adult female outcomes. J Clin Child Adolesc Psychol. 2017;46(4):588–99.
Infurna MR, Fuchs A, Fischer-Waldschmidt G, Reichl C, Holz B, Resch F, et al. Parents’ childhood experiences of bonding and parental psychopathology predict borderline personality disorder during adolescence in offspring. Psychiatry Res. 2016;246:373–8.
Crawford TN, Cohen PR, Chen H, Anglin DM, Ehrensaft M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Dev Psychopathol. 2009;21(3):1013–30.
Johnson JG, Cohen P, Chen H, Kasen S, Brook JS. Parenting behaviors associated with risk for offspring personality disorder during adulthood. Arch Gen Psychiatry. 2006;63(5):579–87.
Schuppert HM, Albers CJ, Minderaa RB, Emmelkamp PMG, Nauta MH. Severity of borderline personality symptoms in adolescence: relationship with maternal parenting stress, maternal psychopathology, and rearing styles. J Pers Disord. 2015;29(3):289–302.
Musser N, Zalewski M, Stepp S, Lewis J. A systematic review of negative parenting practices predicting borderline personality disorder: Are we measuring biosocial theory’s ‘invalidating environment’? Clin Psychol Rev. 2018;65(January):1–16. Available from: https://doi.org/10.1016/j.cpr.2018.06.003
Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. J Consult Clin Psychol. 2002;70(5):1086–98. https://doi.org/10.1037//0022-006X.70.5.1086 .
Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38.
Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006;74(3):489–99. https://doi.org/10.1037/0022-006X.74.3.489 .
Owens EB, Zalecki C, Gillette P, Hinshaw SP. Girls with childhood ADHD as adults: Cross-domain outcomes by diagnostic persistence. J Consult Clin Psychol. 2017;85(7):723–36. https://doi.org/10.1037/ccp0000217 .
Swanson JM. Assessment and treatment of ADD students. Irvine: K.C. Press; 1992.
MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56(12):1073–86.
Bussing R, Fernandez M, Harwood M, Hou Wei, Garvan CW, Eyberg SM, et al. Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment. 2008;15(3):317–28.
Osterrieth PA. The test of copying a complex figure: A contribution to the study of perception and memory. Arch Psychol (Geneve). 1944;30:286–356.
Miller M, Nevado-Montenegro AJ, Hinshaw SP. Childhood executive function continues to predict outcomes in young adult females with and without childhood-diagnosed ADHD. J Abnorm Child Psychol. 2012;40(5):657–68. https://doi.org/10.1007/S10802-011-9599-Y .
Sami N, Carte ET, Hinshaw SP, Zupan BA. Performance of girls with ADHD and comparison girls on the Rey-Osterrieth Complex Figure: evidence for executive processing deficits. Child Neuropsychol. 2003;9(4):237–54. https://doi.org/10.1076/CHIN.9.4.237.23514 .
Hinshaw SP, Carte ET, Sami N, Treuting JJ, Zupan BA. Preadolescent girls with attention-deficit/hyperactivity disorder: II. Neuropsychological performance in relation to subtypes and individual classification. J Consul Clin Psychol. 2002;70(5):1099–111. https://doi.org/10.1037/0022-006X.70.5.1099 .
Achenbach TM. Manual for the child behavior checklist and revised child behavior profile. Burlington, VT: University Associates in Psychiatry; 1991.
Achenbach TM, Rescorla LA. Manual for the ASEBA adult forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2003.
Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the Child Behavior Checklist DSM-oriented scales. J Psychopathol Behav Assess. 2009;31(3):178–89.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–71.
Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory. San Antonio, TX. San Antonio, TX: Psychological Corporation; 1996.
Sprinkle SD, Lurie D, Insko SL, Atkinson G, Jones GL, Logan AR, et al. Criterion validity, severity cut scores, and test-retest reliability of the Beck Depression Inventory-II in a university counseling center sample. J Couns Psychol. 2002;49(3):381–5.
Abidin RR. Parenting Stress Index (PSI) manual. 3rd ed. Charlottesville, VA: Pediatric Psychology Press; 1995.
Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. J Clin Child Adolesc Psychol. 2006;35(2):302–12.
Abidin RR, Brunner JF. Development of a parenting alliance inventory. J Clin Child Psychol. 1995;24(1):31–40.
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–58.
Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abus Negl. 2019;97:104127.
Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45(2):260–73.
Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28(7):729–37.
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, research version, non-patient edition (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 2002.
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV Personality Disorders (SCID–II). Washington, D.C.: American Psychiatric Press; 1997.
Huprich SK, Paggeot AV, Samuel DB. Comparing the Personality Disorder Interview for DSM-IV (PDI-IV) and SCID-II borderline personality disorder scales: an item-response theory analysis. J Pers Assess. 2015;97(1):13–21.
Hopwood CJ, Morey LC, Edelen MO, Shea MT, Grilo CM, Sanislow CA, et al. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychol Assess. 2008;20(1):81–5.
First MB, Williams JB, Benjamin LS, Spitzer RL. Structured clinical interview for DSM-5® personality disorders (SCID-5-PD): With the structured clinical interview for DSM-5® Screening Personality Questionnaire (SCID-5-SPQ). Arlington, VA: American Psychiatric Association; 2016.
Hyland P, Karatzias T, Shevlin M, Cloitre M. Examining the discriminant validity of complex posttraumatic stress disorder and borderline personality disorder symptoms: Results from a United Kingdom population sample. J Trauma Stress. 2019;32(6):855–63.
Frost R, Murphy J, Hyland P, Shevlin M, Ben-Ezra M, Hansen M, et al. Revealing what is distinct by recognising what is common: distinguishing between complex PTSD and Borderline Personality Disorder symptoms using bifactor modelling. Eur J Psychotraumatol. 2020;11:1836864.
Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80(1):27–38.
Kraemer HC. Discovering, comparing, and combining moderators of treatment on outcome after randomized clinical trials: A parametric approach. Stat Med. 2013;32:1964–73.
Meza JI, Owens EB, Hinshaw SP. Childhood predictors and moderators of lifetime risk of self-harm in girls with and without attention-deficit/hyperactivity disorder. Dev Psychopathol. 2021:1–17. https://doi.org/10.1017/S0954579420000553 .
Stepp SD, Scott LN, Jones NP, Whalen DJ, Hipwell AE. Negative emotional reactivity as a marker of vulnerability in the development of borderline personality disorder symptoms. Dev Psychopathol. 2016;28(1):213.
Danese A, Widom CS. Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nat Hum Behav. 2020;4(8):811–8.
Ahmad SI, Hinshaw SP. Attention-Deficit/Hyperactivity Disorder, Trait impulsivity, and externalizing behavior in a longitudinal sample. J Abnorm Child Psychol. 2017;45(6):1077–89.
Perepletchikova F, Nathanson D, Axelrod SR, Merrill C, Walker A, Grossman M, et al. Randomized clinical trial of Dialectical Behavior Therapy for preadolescent children with disruptive mood dysregulation disorder: Feasibility and outcomes. J Am Acad Child Adolesc Psychiatry. 2017;56(10):832–40.
Luby JL, Barch DM, Whalen D, Tillman R, Freedland KE. A randomized controlled trial of parent-child psychotherapy targeting emotion development for early childhood depression. Am J Psychiatry. 2018;175(11):1102–10.
Zalewski M, Maliken AC, Lengua LJ, Gamache Martin C, Roos LE, Everett Y. Integrating dialectical behavior therapy with child and parent training interventions: A narrative and theoretical review. Clin Psychol Sci Pract. 2020; Advance online publication. https://doi.org/10.1111/cpsp.12363 .
Adhikary AC, Rahman MS. Firth’s penalized method in Cox proportional hazard framework for developing predictive models for sparse or heavily censored survival data. J Stat Comput Simul. 2021;91(3):445–63.
Yen S, Peters JR, Nishar S, Grilo CM, Sanislow CA, Shea MT, et al. Association of borderline personality disorder criteria with suicide attempts: Findings from the Collaborative Longitudinal Study of Personality Disorders over 10 years of follow-up. JAMA Psychiat. 2020;02115(2):187–94.
Snyder HR, Miyake A, Hankin BL. Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Front Psychol. 2015;6:328.
Davies SR, Field AR, Andersen T, Pestell C. The ecological validity of the Rey-Osterrieth Complex Figure: Predicting everyday problems in children with neuropsychological disorders. J Clin Exp Neuropsychol. 2011;33(7):820–31.
Weber RC, Riccio CA, Cohen MJ. Does Rey Complex Figure copy performance measure executive function in children? Appl Neuropsychol Child. 2013;2(6–12). https://doi.org/10.1080/09084282.2011.643964 .
McLaughlin KA, Sheridan MA. Beyond cumulative risk: A dimensional approach to childhood adversity. Curr Dir Psychol Sci. 2016;25(4):239–45.
Download references

Acknowledgements
We express gratitude to the young women who have participated in our ongoing investigation, and their families, as well as the members of the Hinshaw lab both past and present who have made this research possible.
Preparation of this research was supported by Grant R01 MH45064 from the National Institute of Mental Health.
Author information
Authors and affiliations.
Department of Psychology, University of California, Berkeley, 2121 Berkeley Way West, Berkeley, CA, 94720-1650, USA
Sinclaire M. O’Grady & Stephen P. Hinshaw
Department of Psychiatry and Behavioral Sciences, University of California, 675 18th Street, San Francisco, San Francisco, CA, 94107, USA
Stephen P. Hinshaw
You can also search for this author in PubMed Google Scholar
Contributions
S.M.O. played a lead role in conceptualization and data curation, formal analysis, writing of original draft, and writing of review and editing. S. P. H. played lead role in the original study design, methodology, data collection, as well as supervision of S. M. O., and an equal contribution in the conceptualization, drafting, and critical revision of this work and writing. All authors read and approved the final manuscript.
Authors’ information
S. M. O. is a psychology doctoral student at the University of California, Berkeley studying developmental pathways to self-harm, with emphasis on trait impulsivity, childhood maltreatment, emotion dysregulation, and suicide. S. P. H. is a Distinguished Professor of Psychology at the University of California, Berkeley, and Professor of Psychiatry and Behavioral Sciences at the University of California, San Francisco. He investigates developmental psychopathology and mental illness stigma.
Corresponding author
Correspondence to Sinclaire M. O’Grady .
Ethics declarations
Ethics approval and consent to participate.
This study and its experimental protocols were approved by the ethics committee at the University of California Berkeley’s Committee for Protection of Human Subjects. All methods were performed in accordance with the relevant guidelines and regulations of the Declaration of Helsinki. Written informed consent was obtained from all participants. Written informed consent was obtained from all participants’ parents/legal guardians if their age was less than 16 years. Written informed consent was obtained from parents/legal guardians and participants for vulnerable participants.
Consent for publication
Not applicable.
Competing interests
All authors have no conflicts of interest to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
O’Grady, S.M., Hinshaw, S.P. Developmental predictors of young adult borderline personality disorder: a prospective, longitudinal study of females with and without childhood ADHD. BMC Psychiatry 23 , 106 (2023). https://doi.org/10.1186/s12888-023-04515-3
Download citation
Received : 25 September 2022
Accepted : 02 January 2023
Published : 15 February 2023
DOI : https://doi.org/10.1186/s12888-023-04515-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Attention-deficit hyperactivity disorder
- Risk factors
- Longitudinal studies
- Adverse childhood experiences
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 March 2022
Borderline personality disorder: associations with psychiatric disorders, somatic illnesses, trauma, and adverse behaviors
- Ashley E. Tate ORCID: orcid.org/0000-0002-4523-6960 1 ,
- Hanna Sahlin ORCID: orcid.org/0000-0002-6353-024X 2 ,
- Shengxin Liu 1 ,
- Yi Lu ORCID: orcid.org/0000-0001-9933-3654 1 ,
- Sebastian Lundström 3 , 4 ,
- Henrik Larsson 1 , 5 ,
- Paul Lichtenstein ORCID: orcid.org/0000-0003-3037-5287 1 &
- Ralf Kuja-Halkola 1
Molecular Psychiatry volume 27 , pages 2514–2521 ( 2022 ) Cite this article
13k Accesses
18 Citations
9 Altmetric
Metrics details
- Bipolar disorder
Psychiatric disorders
- Schizophrenia
In one of the largest, most comprehensive studies on borderline personality disorder (BPD) to date, this article places into context associations between this diagnosis and (1) 16 different psychiatric disorders, (2) eight somatic illnesses, and (3) six trauma and adverse behaviors, e.g., violent crime victimization and self-harm. Second, it examines the sex differences in individuals with BPD and their siblings. A total of 1,969,839 Swedish individuals were identified from national registers. Cumulative incidence with 95% confidence intervals (CI) was evaluated after 5 years of follow-up from BPD diagnosis and compared with a matched cohort. Associations were estimated as hazard ratios (HR) with 95% CIs from Cox regression. 12,175 individuals were diagnosed with BPD (85.3% female). Individuals diagnosed with BPD had higher cumulative incidences and HRs for nearly all analyzed indicators, especially psychiatric disorders. Anxiety disorders were most common (cumulative incidence 95% CI 33.13% [31.48–34.73]). Other notable findings from Cox regressions include psychotic disorders (HR 95% CI 24.48 [23.14–25.90]), epilepsy (3.38 [3.08–3.70]), violent crime victimization (7.65 [7.25–8.06]), and self-harm (17.72 [17.27–18.19]). HRs in males and females with BPD had overlapping CIs for nearly all indicators. This indicates that a BPD diagnosis is a marker of vulnerability for negative events and poor physical and mental health similarly for both males and females. Having a sibling with BPD was associated with an increased risk for psychiatric disorders, trauma, and adverse behaviors but not somatic disorders. Clinical implications include the need for increased support for patients with BPD navigating the health care system.
Similar content being viewed by others

Suicidal behavior across a broad range of psychiatric disorders
Latent profile analysis identifies four different clinical schizophrenia profiles through aberrant salience
Effects of sex and gender on the etiologies and presentation of select internalizing psychopathologies
Introduction.
Borderline Personality Disorder (BPD; Diagnostic and Statistical Manual of Mental Disorders [DSM] terminology), or Emotionally Unstable Personality Disorder (International Classification of Diseases [ICD] terminology), is a serious psychiatric disorder estimated to affect 1.7% of the worldwide population [ 1 ]. The core features of this diagnosis include: unstable interpersonal relationships, recurring self-harm, and emotional dysregulation [ 2 ].
Receiving a BPD diagnosis has been repeatedly associated with a high degree of psychiatric and somatic comorbidities, traumatic events, and criminal behavior [ 3 , 4 , 5 ]. These results have shaped the clinical perception and research directions of BPD, however specific estimates across psychiatric disorders, somatic illnesses, trauma, and adverse behavior have never been comprehensively presented in one study. Moreover, the majority of past studies were limited to smaller clinical samples or cross-sectional community samples, which did not allow for unselected samples nor longitudinal data. Additional longitudinal trait-based epidemiological studies have examined BPD symptoms in twins, however, few participants reached the full diagnostic criteria and thus may not be reflective of individuals with severe BPD symptoms [ 6 , 7 ]. Therefore, it is of interest to examine these estimates in a representative and well-powered population-based study in order to provide the context for a BPD diagnosis and reframe misconceptions.
Psychiatric comorbidities are the rule rather than the exception in patients with BPD. A Swedish national study reported that 95.7% of individuals with a BPD diagnosis had a comorbid psychiatric diagnosis [ 8 ]. Mood disorders, post-traumatic stress disorder (PTSD), impulsive disorders, and bipolar disorders are commonly associated with BPD symptoms and diagnosis [ 9 , 10 , 11 ]. Precise estimates for these comorbidities are lacking, especially for rare and serious disorders, e.g., psychotic disorders [ 12 ].
Somatic illnesses
Individuals with BPD use health care services at a higher rate than those with other personality disorders, and even elevated BPD symptoms are associated with receiving disability [ 13 , 14 ]. BPD has been linked to poor somatic health, such as obesity, diabetes, gastrointestinal disease, cardiovascular disease, hypertension, chronic pain, and sexually transmitted infections [ 3 , 15 ]. It is likely that somatic illnesses associated with BPD have been overlooked in smaller studies, for example, infertility [ 16 , 17 ]. Moreover, patients often perceive the severity of their illness worse than reports based on medical records, highlighting the importance of objective measurement [ 18 ].
Trauma and adverse behaviors
Up to 90% of patients with BPD are estimated to have a history of childhood trauma [ 1 ]. BPD has been linked to an increased risk for sexual abuse victimization in adulthood [ 19 ] and physical trauma resulting from accidents [ 3 ]. However, the association between BPD and other trauma types, e.g., death of a family member, is unclear. The relationship between trauma and BPD is theorized to be bidirectional, although the evidence for this is conflicting [ 20 ]. Similar to somatic reports, capturing objective measures of trauma would prevent biases that may arise from self-reports [ 21 ].
The association between violent crime and a BPD diagnosis is well documented, however less literature exists on nonviolent offenses [ 22 ]. It is unclear which nonviolent offenses are predominant in patients with BPD, although it is likely borne from impulsive actions. As recurrent self-harm is a core feature of BPD [ 2 ], we expect the rate of self-harm requiring medical attention to be higher than the general population. However, a precise estimate from a population sample is unknown.
Sex differences
BPD is predominately diagnosed in females, although evidence suggests that this is largely the result of a diagnostic bias [ 23 ]. Moreover, gender differences have been found for symptom expression and comorbidities [ 22 ]. Males have a higher prevalence of substance use disorders and antisocial personality disorder and exhibit symptoms related to aggression; while females show increased rates of risky behavior and an increased prevalence of comorbid mood disorders, eating disorders, and PTSD [ 22 , 24 ]. Males are typically underrepresented in BPD studies, thus potential differences in outcomes and precursors of BPD is of particular importance. Given a diagnostic bias, males would need greater symptom severity in order to be diagnosed, leading to a difference in symptom severity between the sexes. With this, we hypothesize elevated rates across most categories for males with BPD compared to their female counterparts.
Further, this raises etiological questions about the differences between the sexes. With our hypothesis that males with BPD will have more severe symptomatology, we postulate that individuals with a brother diagnosed with BPD will have higher rates of diagnoses and adverse outcomes across all domains compared to those with a sister with a BPD diagnosis, similar to the so-called female protective effect in autism, with the sexes reversed [ 25 ].
Present study
The primary aim of this study was to describe the extent of the association for individuals with BPD and (1) psychiatric disorders, (2) somatic illnesses, and (3) trauma and adverse behaviors in a Swedish nationwide sample. As sensitivity analyses, we examined the temporal order of these associations, sex-specific differences for individuals, and those with siblings diagnosed with BPD.
Materials and methods
Study population.
The study population included individuals born in Sweden between January 1st, 1973 and December 31st, 1993 with a personal identity number and a biological mother identifiable in the register (2,177,075). We excluded individuals with a congenital malformation (113,566), those who died before age 18 (6972), and/or emigrated before age 18 (62,664). Thus, 1,969,839 individuals were included in our study.
Data sources
Swedish personal identity numbers were used to link multiple Swedish registers in order to identify the cohort and create the analyzed variables, termed here as “indicators” (Table 1 ) [ 26 , 27 , 28 , 29 , 30 ]. The National Patient Register (NPR) contains administrative data from in-patient and specialist outpatient care (but not primary care) with diagnosis made by licensed medical doctors. The diagnoses have been externally validated by reviewing a random subset of patient’s medical records with comparison to the received diagnostic code. The positive predictive value of the psychiatric and somatic diagnoses in the register is high; out of the investigated medical records 80% or more retained the stated diagnostic code upon review [ 29 ]. Physical trauma requiring medical attention was found to have an acceptable positive predictive value of 74% [ 30 , 31 ].
BPD diagnosis was defined by receiving an Emotionally Unstable Personality Disorder diagnosis in the NPR (ICD 10th revision: F60.3) by psychiatrists in in- or outpatient psychiatric clinics. In one validation study, structured interviews had been used in 36% of examined personality disorders (including other personality disorders than BPD), as identified from medical charts. However, the positive predictive value, i.e., proportion of diagnoses validated upon review, for the 26 BPD-diagnoses investigated was high regardless if structured interviews had been used or not, between 77% (based on DSM-criteria) and 100% (based on ICD-criteria); inter-rater agreement was between 85% (ICD-criteria) and 100% (DSM-criteria) [ 32 ]. Another validation study based on 70 medical charts with a BPD-diagnosis, and reported a positive predictive value of 81%, with an inter-rater agreement of 93% [ 33 ].
The indicators in our study were selected based on an existing data linkage, which contains a subset of all ICD-codes (Supplementary Table 1 ). Indicators were placed into three groups: psychiatric disorders, somatic illnesses, and trauma and adverse behaviors (Supplementary Tables 2 – 4 ). As a sensitivity analysis, we analyzed the three most common subcategories for umbrella indicators with many subtypes, e.g., autoimmune disorders. Adverse behaviors included violent/nonviolent crime and self-harm. Trauma included accidents requiring medical attention, violent crime victimization requiring medical attention, death of a close family member, and childhood neighborhood quality.
We only considered time of the first observed event for all indicators, except for childhood poverty and neighborhood quality.
The study was approved by the Regional Ethics Committee in Stockholm, Sweden (Dnr 2013/862 31/5). As our study participants were non-identifiable, no informed consent was needed by Swedish law.
Statistical analysis
Cumulative incidence.
First, we estimated cumulative incidence for those with and without a BPD diagnosis in order to quantify the associations between BPD and the indicators on an absolute scale. Each patient with BPD was matched with ten individuals not diagnosed with BPD on birth year and sex. Follow up for individuals with BPD began at the date of the first observed BPD diagnosis and continued until the end of follow-up, December 31, 2013, this date was also used for their matched non-exposed individuals. We calculated 5-year cumulative incidence, interpreted as the probability of the event occurring within 5 years, while accounting for censoring. We used Kaplan-Meier estimation to estimate the cumulative incidence as 1 minus the survival function.
Associations between BPD diagnosis and the indicators
To quantify the association between BPD and our indicators, hazard ratios (HR) with 95% confidence intervals (CI) were obtained using sex-stratified Cox regression. Age was used as an underlying time score and we adjusted for birth cohort (1973–1977, 1978–1982, 1983–1987, and 1988–1993). BPD diagnosis was treated as a binary, time-constant, exposure regardless of when the diagnosis occurred. We followed each individual from birth or the start of ICD-9, January 1, 1987, until the first instance of either death, emigration, indicator occurrence, or end of follow-up. We did not account for competing risks, since standard methods introduce changes in the association dependent on whether the exposure is associated with the competing outcome [ 34 ].
We adjusted the analysis for multiple testing according to Benjamini–Hochberg method, with an alpha of 0.05, we obtained a false discovery rate p value threshold of 8.34 · 10 −58 for the main analysis and 0.04 for secondary analyses [ 35 ].
Secondary analyses
Sex-separated and sibling analysis.
To evaluate potential differences between males and females diagnosed with BPD, we repeated the cumulative incidence-, association-, and time-varying analyses by analyzing males and females separately. To investigate potential etiological differences, we repeated the association analyses among men and women separately, split by exposure being having a full sister or having a full brother with a BPD diagnosis.
Time-varying sensitivity analyses
By not considering timing of exposure in our main analysis, we assumed that individuals were exposed since birth although the BPD diagnosis occurred at a later age. This means that we were “borrowing information from the future”, an approach that may introduce bias. Therefore, we repeated all Cox regression analyses comparing the indicators before or after a BPD diagnosis to treat exposures as time-varying. Risk factor analyses considered the indicators to be exposures prior to a BPD diagnosis, while outcome analyses considered indicators as an outcome following a BPD diagnosis.
SAS was used for data management and all subsequent analysis was done in R using the survival package [ 36 ].
Descriptive statistics
The cohort consisted of 1,969,839 individuals (48.8% female) with 12,175 individuals with BPD (85.3% female; 0.6% of sample) (Table 2 ; absolute values Supplementary Tables 5 – 7 ). Total follow-up time was 32,637,932 person-years, calculated from the first possible time of BPD diagnosis, i.e., from its introduction in 1997, and onward. The diagnosis was evenly distributed between birth year cohorts, and the total cohort had a mean age of 29.69 years at the end of follow-up.
Cumulative incidences
The 5-year cumulative incidence showed increased incidences in individuals with BPD compared to the matched control sample for all indicators, except intellectual disability (Fig. 1 ; Supplementary Figs. 1 – 7 ). The largest cumulative incidences were for anxiety disorders (Cumulative incidence [95% CI]; BPD 33.13% [31.48–34.73%]; not BPD (NBPD) 3.17% [2.98–3.79%]), major depressive disorder (BPD 25.65% [24.11–27.16%]; NBPD 3.04% [2.85–3.24%]) personality disorders (BPD 21.33% [20.26–22.39%]; NBPD 0.36% [0.31–0.41%]), accidents requiring medical attention (BPD 21.50% [20.13–22.64%]; NBPD 10.91% [10.60–11.21%]), and attention-deficit hyperactive disorder (BPD 14.62% [13.75–15.48%]; NBPD 0.81% [0.74–0.88%]). Intellectual disability had zero first event occurrences after date of BPD-diagnosis for both exposed and unexposed.
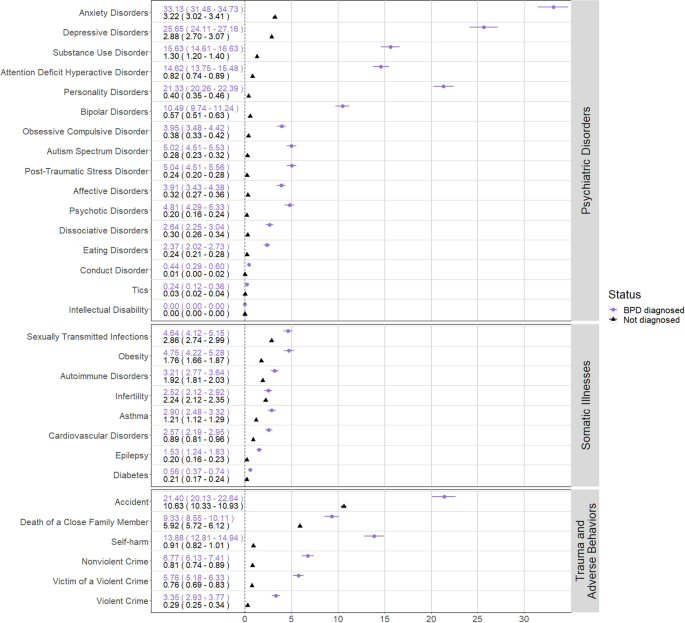
The cumulative incidence of each of the main indicators broken down by subgroups.
Associations between BPD diagnosis and indicators
All HRs for BPD and the indicators included in our main analysis were statistically significant, i.e., larger than 1, after correcting for multiple testing, except for intellectual disability and infertility in females (Fig. 2 ). The majority of the indicators under the umbrella categories were also statistically significantly larger than 1 (Supplementary Figs. 8 and 9 ).
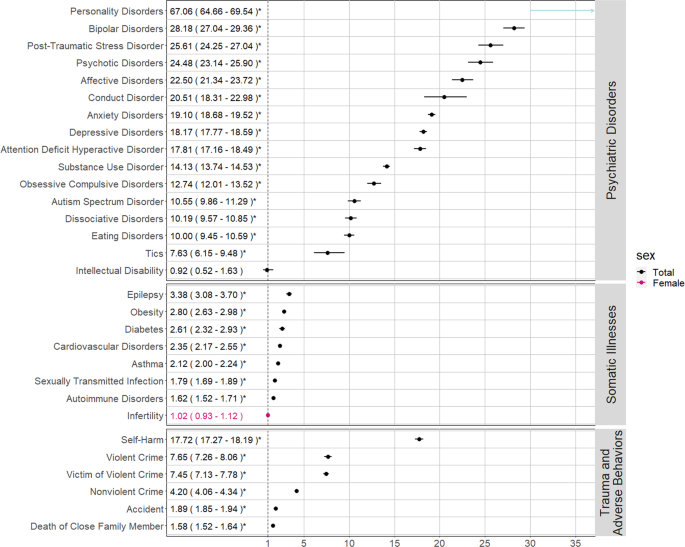
*Statistically significant after correcting for multiple testing using the Benjamini-Hochberg method, resulting in a p value threshold of 8.34 · 10 −58 .
Psychiatric disorders had the highest HRs across all analyses. The highest HRs were personality disorders not including BPD (HR [95% CI] 67.06 [64.66–69.54]), bipolar disorders (28.18 [27.04–29.36]), and PTSD (25.61 [24.25–27.04]). Psychotic disorders were also elevated (24.48 [23.14–25.90]).
The largest HRs for the association between BPD and somatic illnesses were for epilepsy (3.38 [3.08–3.70]), obesity (2.8 [2.63–2.98]), and diabetes (2.61 [2.32–2.93]).
Traumatic events and adverse behaviors
The strongest association regarding traumatic events was violent crime victimization (7.45 [7.13–7.78]). Death of a close family member also had a positive association (1.58 [1.52–1.64]). Self-harm had the highest hazard ratios of adverse behaviors (17.72 [17.27–18.19]). Committing a violent crime (7.65 [7.26–8.06]) had a stronger association than nonviolent crimes (4.20 [4.06–4.34]). Impulsive nonviolent crimes, i.e., property damage (6.66 [6.05–7.33]), had a stronger association than planned crime, possessing fake identification (1.94 [1.19–3.17]). Although they were analyzed as risk factors by definition, the HRs for poverty in childhood (1.93 [1.86–2.00]) and childhood neighborhood quality (1.52 [1.47–1.59]) were positively associated with BPD diagnosis (Supplementary Fig. 10 and Supplementary Table 5 ).
Females with BPD had higher cumulative incidences compared to males with BPD in nearly all somatic disorders, e.g., obesity (male 1.80 [0.97–2.62]; female 5.29 [4.68–5.90]); while the inverse was true for adverse behaviors and traumas, e.g., committing a violent crime (male 10.27 [8.14–12.35]; female 2.44 [2.06–2.83]). However, the CIs frequently overlapped between the sexes (Supplementary Figs. 11 – 23 ). HRs were largely uniform (Supplementary Fig. 24 ). Males had higher HRs for bipolar disorder (male 36.31 [32.62–40.41]; female 27.11 [25.93–28.33]), PTSD (male 34.99 [29.54–41.44], female 24.72 [23.35–26.18]) and affective disorders (male 31.42 [27.63–35.72]; female 21.32 [20.13–22.59]). Somatic disorders were mostly uniform across sex. Committing a violent crime was relatively more elevated in females (male 6.90 [6.38–7.46]; female 8.25 [7.68–8.86]). Additionally, being a victim of a violent crime requiring medical attention had a higher HR in females (male 5.05 [4.56–5.58]; female 8.58 [8.17–9.01]).
Individuals with siblings diagnosed with BPD had increased rates of indicators, however, many CIs contained 1, especially within somatic disorders (Supplementary Tables 9 – 11 ). Individuals with brothers diagnosed with BPD had higher HRs than those with sisters who were diagnosed in 87 out of 123 indicators. Psychiatric disorders had the strongest association, e.g., PTSD (males with brothers diagnosed with BPD (BBPD) 6.76 [3.74–12.24], males with sisters diagnosed with BPD (SBPD) 2.62 [1.78–3.87], females with BBPD 4.09 [2.72–6.16], females with SBPD 3.62 [3.02–4.35]).
Broadly, the magnitude of HRs for each indicator stayed relatively consistent when treating indicators as a risk factor prior to, or as an outcome following, a BPD diagnosis (Supplementary Tables 8 , 12 – 13 and Supplementary Figs. 10 , 25 , and 26 . Some notable exceptions were personality disorders (HR [95% CI] risk factor for subsequent BPD diagnosis 71.50 [68.36–74.78]; outcome following a BPD diagnosis 43.77 [41.40–46.28]), bipolar disorders (risk 35.94 [34.16–37.82]; outcome 17.27 [16.12–18.51), and psychotic disorders (risk 25.82 [24.19–27.56]; outcome 17.96 [16.23–19.87]) which had higher HRs leading up to a BPD diagnosis, and epilepsy (risk 2.89 [2.59–3.22]; outcome 5.36 [4.53–6.34]) that had a higher HR following a BPD diagnosis.
In this population-based study, which included 12,175 individuals with BPD in a total sample of 1,969,839 Swedes, we found that BPD was associated with an increased risk for psychiatric comorbidities, somatic illnesses, traumatic events, and adverse behaviors. Our findings replicate previously known associations and identify unknown or understudied associations, e.g., epilepsy, infertility, and death of close family members. Moreover, this work extends findings to include both sexes and their siblings.
BPD was strongly associated with all psychiatric disorders except intellectual disability. We found a robust association between BPD and all other personality disorders, mood disorders, eating disorders, PTSD, and substance use disorders. Certain findings need additional vigilance from clinicians and researchers, e.g., the strong association with psychotic disorders. This finding follows the historical implication of the term borderline, coined to indicate that the patients were on the borderline between psychosis and neurosis [ 37 ]. Psychotic experiences are often treated as transient symptoms according to DSM guidelines, although symptoms are often perpetual [ 12 ]. Our finding highlights the importance of carefully assessing psychotic symptoms in BPD, and indicates that psychotic disorders are indeed overrepresented in individuals with BPD [ 38 ].
Individuals with BPD had a higher risk of almost all somatic comorbidities in the main analysis except for female infertility. A Danish study also found a positive association between somatic disorders and combined personality disorders, however, their estimates were smaller than our results [ 39 ]. This could suggest that a BPD diagnosis has a worse prognosis than other personality disorders. In line with the literature, epilepsy and metabolic-related comorbidities, such as type 2 diabetes and obesity, had the strongest associations [ 10 ]. Previous studies have indicated a relationship between epilepsy and BPD, and here we show a clear association [ 40 ].
Individuals with BPD were at a higher risk of all traumatic events both before and after receiving their diagnosis. Namely, individuals with BPD were at a higher risk of seeking medical care due to violent crime victimization, especially sexual assault, which had the strongest association. This supports the expansive literature linking sexual assault and a BPD diagnosis [ 19 ]. Second, there was a positive association between BPD and the death of a close family member, which has only been reported in studies involving the death of a parent in childhood [ 41 ]. Third, our study identified an underreported positive link between childhood poverty and poor neighborhood quality and subsequent BPD diagnosis [ 42 ]. Although the CIs overlapped, sex-separated analysis found that males had higher rates of traumatic events, except for sexual assault, fitting within previous literature on BPD symptoms and trauma [ 43 ].
The consistent time-varying results provide evidence for the theory of a close, cyclical relationship between trauma and BPD [ 1 , 20 ]. Our sibling analysis found evidence to support an overlap in genetic and/or environmental etiology between traumatic events and BPD diagnosis, previously theorized to be present [ 44 ].
As expected, BPD individuals had higher instances of adverse behaviors: self-harm, violent and nonviolent crime. In line with previous findings, the most common criminal behaviors were aggressive in nature, such as making violent threats and assault [ 2 , 4 ]. Additionally, our study identified that impulsive nonviolent crimes such as property damage or petty theft are more common than planned crimes, e.g., having fake identification.
Sex differences and time-varying findings
The HRs were largely uniform across sexes, even though the absolute proportions, i.e., cumulative incidences, sometimes differed substantially. This suggests that this disorder confers similar increase in rates of comorbidities between males and females. A diagnostic bias between the sexes could result in an inflated estimate for males with BPD, as males who receive the correct diagnosis might have a more severe symptom presentation.
Individuals with a sibling with BPD had higher rates of psychiatric disorders, trauma, and adverse behaviors but not somatic disorders. HRs were higher in individuals with a brother diagnosed with BPD compared to those with a sister diagnosed for the majority of indicators. Families with a male diagnosed with BPD appear to have a more severe phenotype and vulnerability to psychiatric disorders [ 45 ]. However, this must be interpreted with caution as the CIs overlapped for having a brother or sister diagnosed with BPD. Follow-up on these associations is needed.
As the associations for the time-varying analyses were largely consistent with the main analysis, ignoring time of BPD diagnosis did not introduce bias that invalidated our inferences.
Strengths, weaknesses
In the largest and most detailed BPD study to date, we were able to capture all Sweden-born individuals with BPD with prospective follow-up using national records. This considerable sample size allowed us to thoroughly examine a variety of understudied variables in a representative sample.
However, this study comes with caveats. First, although the NPR and BPD diagnostic codes are well-validated, the extent to which these comorbidities may be misdiagnosed is unclear [ 29 , 32 , 33 ]. However, one may argue that diagnoses, if not correctly diagnosed, may reflect levels of symptom presentation even if the full criteria of diagnosis is not met. Further, the prevalence of a BPD diagnosis in our sample (0.6%) is conservative compared to the projected median estimate of 1.7% [ 1 ]. This likely indicates that many individuals who meet the criteria for a BPD diagnosis remain undiagnosed. And, as a BPD diagnosis generally takes multiple, intensive clinical interviews, it is likely that we are capturing individuals with more severe BPD symptoms.
Next, we were only able to identify the instances of the indicators identifiable in the register, this means the true estimate of these incidences may be higher in under-reported or less severe cases. Some individuals with BPD may be less willing to seek certain types of medical care due to distrust or stigmatization from the health care system, which may attenuate our results [ 46 ]. Additionally, trauma is both an objective and deeply subjective experience; and we are unable to capture the subjective experience [ 21 ]. Finally, symptoms of BPD, like all psychiatric disorders, are continuously distributed across the population rather than a binary diagnosis. We are unable to examine specific BPD symptoms which limits the information gained from this study.
Future directions for research
This study identifies many avenues for needed research. The comorbidities between BPD and psychotic disorders should be examined further. Moreover, the association with death of a close family member opens the question of the heritability of premature mortality in families [ 47 ]. Also, studies should examine these associations in other severe psychiatric disorders, such as bipolar disorder, to determine what associations are specific to BPD rather than general to severe psychiatric disorders [ 48 , 49 ]. Finally, further research should carefully expand on any causal assumptions about the nature of BPD.
Clinical implications
Our results indicate individuals with BPD frequently use health care services for a variety of psychiatric and somatic conditions. Unfortunately, despite their needs, the interpersonal difficulties and stigma surrounding individuals with BPD can be challenging for clinicians, which often results in poor care or premature ending of treatment [ 46 , 50 ]. Thus, there is a clear need for support and advocates for individuals with BPD navigating the health care system. Clinicians should be aware of these difficulties within the health care system and offer adapted health education or referrals, e.g., a dietitian to prevent type 2 diabetes. Additionally, implementing already developed anti-stigmatization methods could help improve the doctor–patient relationship [ 50 , 51 ].
Conclusions
BPD was associated with nearly all of the more than 30 indicators of psychiatric disorders, somatic illnesses, trauma, and adverse behavior. The associations were consistent across sex and temporality. This paper can serve as an atlas for associations within the aforementioned categories, many of which have previously been un- or under-reported, and can lead the way towards further causal and etiological research. Critically, the clinical implications indicate that increased support is needed for patients surrounding health care visits. It is hopeful that this provides the groundwork towards an understanding and increased awareness for this patient group.
Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Prim. 2018;4:1–20.
Google Scholar
APA. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Association Publication; 2013.
Frankenburg FR, Zanarini MC. The association between borderline personality disorder and chronic medical illnesses, poor health-related lifestyle choices, and costly forms of health care utilization. J Clin Psychiatry . 2004.
Arola R, Antila H, Riipinen P, Hakko H, Riala K, Kantojärvi L. Borderline personality disorder associates with violent criminality in women: a population based follow-up study of adolescent psychiatric inpatients in Northern Finland. Forensic Sci Int. 2016;266:389–95.
Article PubMed Google Scholar
Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry. 2004;161:2108–14.
Czajkowski N, Aggen SH, Krueger RF, Kendler KS, Neale MC, Knudsen GP, et al. A twin study of normative personality and DSM-IV personality disorder criterion counts: evidence for separate genetic influences. Am J Psychiatry. 2018;175:649–56.
Article PubMed PubMed Central Google Scholar
Torgersen S, Czajkowski N, Jacobson K, Reichborn-Kjennerud T, Røysamb E, Neale M, et al. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: a multivariate study. Psychol Med. 2008;38:1617–25.
Article CAS PubMed Google Scholar
Skoglund C, Tiger A, Rück C, Petrovic P, Asherson P, Hellner C, et al. Familial risk and heritability of diagnosed borderline personality disorder: a register study of the Swedish population. Mol. Psychiatry. 2019:1–10.
Zapolski TC, Settles RE, Cyders MA, Smith GT. Borderline personality disorder, bulimia nervosa, antisocial personality disorder, ADHD, substance use: common threads, common treatment needs, and the nature of impulsivity. Independent . Practitioner. 2010;30:20.
Tomko RL, Trull TJ, Wood PK, Sher KJ. Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. J Personal Disord. 2014;28:734–50.
Article Google Scholar
Welander-Vatn A, Ystrom E, Tambs K, Neale M, Kendler K, Reichborn-Kjennerud T, et al. The relationship between anxiety disorders and dimensional representations of DSM-IV personality disorders: a co-twin control study. J Affect Disord. 2016;190:349–56.
Barnow S, Arens EA, Sieswerda S, Dinu-Biringer R, Spitzer C, Lang S. Borderline personality disorder and psychosis: a review. Curr Psychiatry Rep. 2010;12:186–95.
Doering S. Borderline personality disorder in patients with medical illness: a review of assessment, prevalence, and treatment options. Psychosom Med. 2019;81:584–94.
Østby KA, Czajkowski N, Knudsen GP, Ystrom E, Gjerde LC, Kendler KS, et al. Personality disorders are important risk factors for disability pensioning. Soc Psychiatry Psychiatr Epidemiol. 2014;49:2003–11.
El-Gabalawy R, Katz LY, Sareen J. Comorbidity and associated severity of borderline personality disorder and physical health conditions in a nationally representative sample. Psychosom Med. 2010;72:641–7.
Sharma TR. Polycystic ovarian syndrome and borderline personality disorder: 3 case reports and scientific review of literature. J Psychiatry. 2015;18:1–4.
De Genna NM, Feske U, Larkby C, Angiolieri T, Gold MAPregnancies. abortions, and births among women with and without borderline personality disorder. Women’s Health Issues. 2012;22:e371–e377.
Sansone RA, Sansone LA. Borderline personality: a primary care context. Psychiatry. 2004;1:19.
PubMed PubMed Central Google Scholar
de Aquino Ferreira LF, Pereira FHQ, Benevides AMLN, Melo MCA. Borderline personality disorder and sexual abuse: a systematic review. Psychiatry Res. 2018;262:70–77.
Conway CC, Boudreaux M, Oltmanns TF. Dynamic associations between borderline personality disorder and stressful life events over five years in older adults. Personal Disord: Theory Res Treat. 2018;9:521.
Baldwin JR, Degli Esposti M. Triangulating evidence on the role of perceived versus objective experiences of childhood adversity in psychopathology. JCPP Adv. 2021;1:e12010.
Sansone RA, Sansone LA. Gender patterns in borderline personality disorder. Innov Clin Neurosci. 2011;8:16.
Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:533.
Barnow S, Herpertz SC, Spitzer C, Stopsack M, Preuss UW, Grabe HJ, et al. Temperament and character in patients with borderline personality disorder taking gender and comorbidity into account. Psychopathology. 2007;40:369–78.
Robinson EB, Lichtenstein P, Anckarsäter H, Happé F, Ronald A. Examining and interpreting the female protective effect against autistic behavior. Proc Natl Acad Sci. 2013;110:5258–62.
Article CAS PubMed PubMed Central Google Scholar
Källén B, Källén K. The Swedish Medical Birth Register—a summary of content and quality. 2003.
Careja R, Bevelander P. Using population registers for migration and integration research: examples from Denmark and Sweden. Comp Migr Stud. 2018;6:19.
Brooke HL, Talbäck M, Hörnblad J, Johansson LA, Ludvigsson JF, Druid H, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32:765–73.
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim J-L, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450.
Ludvigsson JF, Svedberg P, Olén O, Bruze G, Neovius M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;344:1–15.
Tampe U, Frank S, Weiss RJ, Jansson K-Å. Diagnosis of open tibial fracture showed high positive predictive value in the Swedish National Patient Register. Clin Epidemiol. 2020;12:1113.
Kouppis E, Ekselius L. Validity of the personality disorder diagnosis in the Swedish National Patient Register. Acta Psychiatr Scand. 2020;141:432–8.
Kuja-Halkola R, Juto KL, Skoglund C, Rück C, Mataix-Cols D, Pérez-Vigil A, et al. Do borderline personality disorder and attention-deficit/hyperactivity disorder co-aggregate in families? A population-based study of 2 million Swedes. Mol Psychiatry. 2018:261:1–9.
Bhaskaran K, Rachet B, Evans S, Smeeth L. Re: Helene Hartvedt Grytli, Morten Wang Fagerland, Sophie D. Fosså, Kristin Austlid Taskén. Association between use of β-blockers and prostate cancer-specific survival: a cohort study of 3561 prostate cancer patients with high-risk or metastatic disease. Beta-Blockers and Prostate Cancer Survival-Interpretation of Competing Risks Models. Eur Urol. 2022;64:e86–e87. https://doi.org/10.1016/j.eururo.2013.01.007 .
Article CAS Google Scholar
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc: Ser B (Methodol). 1995;57:289–300.
Therneau T. A package for survival analysis in R. R package version 3.2-3. Computer software] Rochester, MN: Mayo Clinic. https://CRAN.R-project.org/package=survival . 2020.
Slotema CW, Daalman K, Blom JD, Diederen KM, Hoek HW, Sommer I. Auditory verbal hallucinations in patients with borderline personality disorder are similar to those in schizophrenia. Psychological Med. 2012;42:1873.
Strålin P, Hetta J. First episode psychosis: register-based study of comorbid psychiatric disorders and medications before and after. Eur Arch Psychiatry Clin Neurosci. 2020;271:303–13.
Momen NC, Plana-Ripoll O, Agerbo E, Benros ME, Børglum AD, Christensen MK, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. 2020;382:1721–31.
Lanska DJ. The Klüver-Bucy syndrome. Neurologic-psychiatric syndromes in focus—Part I . 41. Karger Publishers; 2018. p. 77–89.
Weaver TL, Clum GA. Early family environments and traumatic experiences associated with borderline personality disorder. J Consulting Clin Psychol. 1993;61:1068.
Cohen P, Chen H, Gordon K, Johnson J, Brook J, Kasen S. Socioeconomic background and the developmental course of schizotypal and borderline personality disorder symptoms. Dev Psychopathol. 2008;20:633–50.
Amstadter AB, Aggen SH, Knudsen GP, Reichborn-Kjennerud T, Kendler KS. Potentially traumatic event exposure, posttraumatic stress disorder, and Axis I and II comorbidity in a population-based study of Norwegian young adults. Soc Psychiatry Psychiatr Epidemiol. 2013;48:215–23.
White CN, Conway CC, Oltmanns TF. Stress and personality disorders. The Oxford handbook of stress and mental health 2019 : 183.
Neale MC, Røysamb E, Jacobson K. Multivariate genetic analysis of sex limitation and G × E interaction. Twin Res Hum Genet. 2006;9:481–9.
Hall K, Moran P. Borderline personality disorder: an update for neurologists. Pract Neurol. 2019;19:483–91.
Temes CM, Frankenburg FR, Fitzmaurice GM, Zanarini MC. Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. 2019;80:0–0.
Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci. 2014;2:119–37.
Kjær JN, Biskin R, Vestergaard C, Munk-Jørgensen P. All-cause mortality of hospital-treated borderline personality disorder: a nationwide cohort study. J Personal Disord. 2020;34:723–35.
Healthcare Management Forum. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum 2017. SAGE Publications Sage CA: Los Angeles, CA.
Knaak S, Szeto AC, Fitch K, Modgill G, Patten S. Stigma towards borderline personality disorder: effectiveness and generalizability of an anti-stigma program for healthcare providers using a pre-post randomized design. Borderline Personal Disord Emot Dysregul. 2015;2:1–8.
Download references
Tate has received funding from the European Union’s Horizon 2020 Research and Innovation Program under the Marie Sklodowska-Curie CAPICE Project grant agreement number 721567. ( https://www.capice-project.eu/ ) Lu is in part supported by a 2018 NARSAD Young Investigator Grant from the Brain & Behaviour Research Foundation and US NIMH (R01 MH123724). Open access funding provided by Karolinska Institute.
Author information
Authors and affiliations.
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Solna, Sweden
Ashley E. Tate, Shengxin Liu, Yi Lu, Henrik Larsson, Paul Lichtenstein & Ralf Kuja-Halkola
Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
Hanna Sahlin
Centre for Ethics, Law and Mental Health (CELAM), University of Gothenburg, Gothenburg, Sweden
Sebastian Lundström
Gillberg Neuropsychiatry Centre, University of Gothenburg, Gothenburg, Sweden
School of Medical Sciences, Örebro University, Örebro, Sweden
Henrik Larsson
You can also search for this author in PubMed Google Scholar
Contributions
AET, RK-H, and HS conceptualized the study. AET completed the analysis and wrote the manuscript. SL, YL, SL, PL, HS, RK-H provided feedback on the conceptualization and manuscript.
Corresponding author
Correspondence to Ashley E. Tate .
Ethics declarations
Competing interests.
Larsson reports: Evolan (speaker); Shire (speaker, grant recipient); Takeda (speaker, grant recipient) all outside the submitted work. Tate, Sahlin, Liu, Lu, Lundström, Lichtenstein, Kuja-Halkola report no financial relationships with commercial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Tate, A.E., Sahlin, H., Liu, S. et al. Borderline personality disorder: associations with psychiatric disorders, somatic illnesses, trauma, and adverse behaviors. Mol Psychiatry 27 , 2514–2521 (2022). https://doi.org/10.1038/s41380-022-01503-z
Download citation
Received : 16 July 2021
Revised : 01 February 2022
Accepted : 22 February 2022
Published : 18 March 2022
Issue Date : May 2022
DOI : https://doi.org/10.1038/s41380-022-01503-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
VIDEO
COMMENTS
Related research continues to evolve into cluster #1 "borderline personality disorder and emotions" (S=0.87; 2007) and cluster #2 "borderline personality disorder and social cognition" (S=0.911; 2009), researchers have focused on understanding the causal relationship between BPD traits and factors such as social environment, emotion ...
Introduction. Borderline personality disorder (BPD) is a severe and heterogeneous mental disturbance connoted by a pattern of identity diffusion, interpersonal disturbances, and chronic instability, with episodes of severe affective and impulsive dyscontrol ().Personality disorders (PD) do not suddenly emerge in the adulthood; in fact, prodromal signs and processes that confer vulnerability to ...
Borderline personality is a serious psychiatric disorder, with a prevalence of about 4% in the community, but as high as 20% in many clinical psychiatric populations, and significant morbidity. It is difficult to treat (both in the sense of responding poorly and as personally troubling to the therapist and the treatment team) and poorly understood.
This review summarizes advances in treatments for adults with borderline personality disorder (BPD) in the last 5 years. ... Papers of Particular Interest, Published recently, Have Been Highlighted as: • Of Importance ... Remen AL. A manual-based psychodynamic therapy for treatment-resistant borderline personality disorder. Psychotherapy ...
Borderline personality disorder can be a difficult diagnosis because of similarities to other conditions, particularly mood disorders. It is a common presentation in both psychiatric and general practice, with accurately diagnosed cases seen in 10% of psychiatric outpatients, 20% of psychiatric inpatients 1, 2 and 6% of family medicine patients. 3 These values are higher than would be expected ...
In 1980, borderline personality disorder (BPD) was introduced in the DSM-III 6, based on a study by Spitzer et al 7, who drew both on research by Gunderson and colleagues 8, 9 and on Kernberg's concept of borderline personality organization 3, by including specific problems of identity and interpersonal relationships characterized by sudden ...
Background Research on the precursors of borderline personality disorder (BPD) reveals numerous child and adolescent risk factors, with impulsivity and trauma among the most salient. Yet few prospective longitudinal studies have examined pathways to BPD, particularly with inclusion of multiple risk domains. Methods We examined theory-informed predictors of young-adult BPD (a) diagnosis and (b ...
Progress in understanding borderline personality disorder has unfolded in the last decade, landing in a new COVID-19-influenced world. Borderline personality disorder is now firmly established as a valid diagnosis, distinct from its co-occurring mood, anxiety, trauma-related, and behavioral disorders. Further, it is also understood as a reflection of general personality dysfunction ...
Borderline personality disorder (BPD) is a mental disorder with a high burden on patients, family members, and health-care systems. The condition was previously regarded as untreatable, but progress in understanding and management has resulted in earlier diagnosis and better treatment outcomes. A coherent syndrome of BPD typically onsets during adolescence (after age 12 years). BPD is often ...
In one of the largest, most comprehensive studies on borderline personality disorder (BPD) to date, this article places into context associations between this diagnosis and (1) 16 different ...