Module 11: Schizophrenia Spectrum and Other Psychotic Disorders
Case studies: schizophrenia spectrum disorders, learning objectives.
- Identify schizophrenia and psychotic disorders in case studies

Case Study: Bryant
Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized thoughts and delusion of control were noticeable. He told the doctors he has not been receiving any treatment, was not on any substance or medication, and has been experiencing these symptoms for about two weeks. Throughout the course of his treatment, the doctors noticed that he developed a catatonic stupor and a respiratory infection, which was identified by respiratory symptoms, blood tests, and a chest X-ray. To treat the psychotic symptoms, catatonic stupor, and respiratory infection, risperidone, MECT, and ceftriaxone (antibiotic) were administered, and these therapies proved to be dramatically effective. [1]
Case Study: Shanta
Shanta, a 28-year-old female with no prior psychiatric hospitalizations, was sent to the local emergency room after her parents called 911; they were concerned that their daughter had become uncharacteristically irritable and paranoid. The family observed that she had stopped interacting with them and had been spending long periods of time alone in her bedroom. For over a month, she had not attended school at the local community college. Her parents finally made the decision to call the police when she started to threaten them with a knife, and the police took her to the local emergency room for a crisis evaluation.
Following the administration of the medication, she tried to escape from the emergency room, contending that the hospital staff was planning to kill her. She eventually slept and when she awoke, she told the crisis worker that she had been diagnosed with attention-deficit/hyperactive disorder (ADHD) a month ago. At the time of this ADHD diagnosis, she was started on 30 mg of a stimulant to be taken every morning in order to help her focus and become less stressed over the possibility of poor school performance.
After two weeks, the provider increased her dosage to 60 mg every morning and also started her on dextroamphetamine sulfate tablets (10 mg) that she took daily in the afternoon in order to improve her concentration and ability to study. Shanta claimed that she might have taken up to three dextroamphetamine sulfate tablets over the past three days because she was worried about falling asleep and being unable to adequately prepare for an examination.
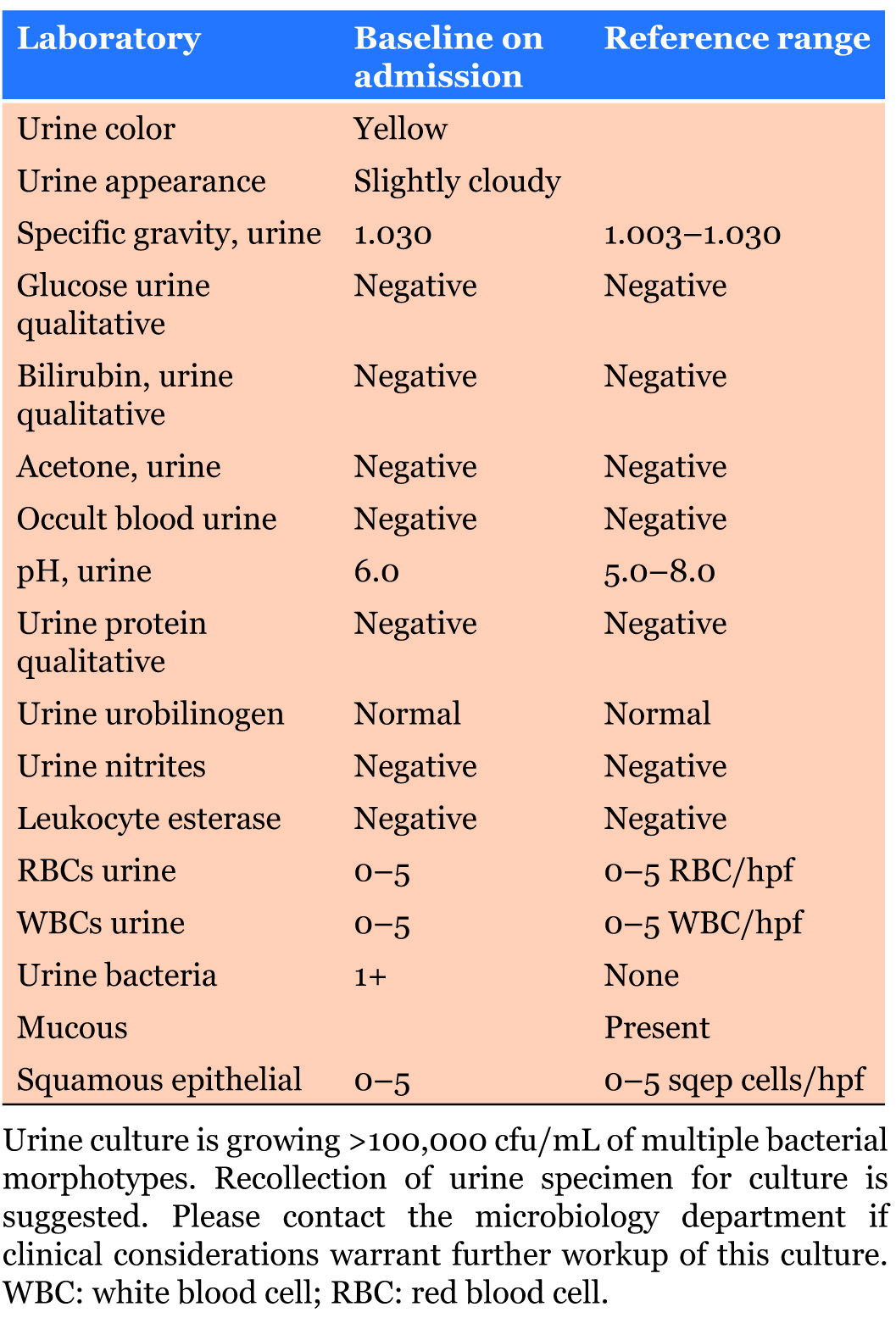
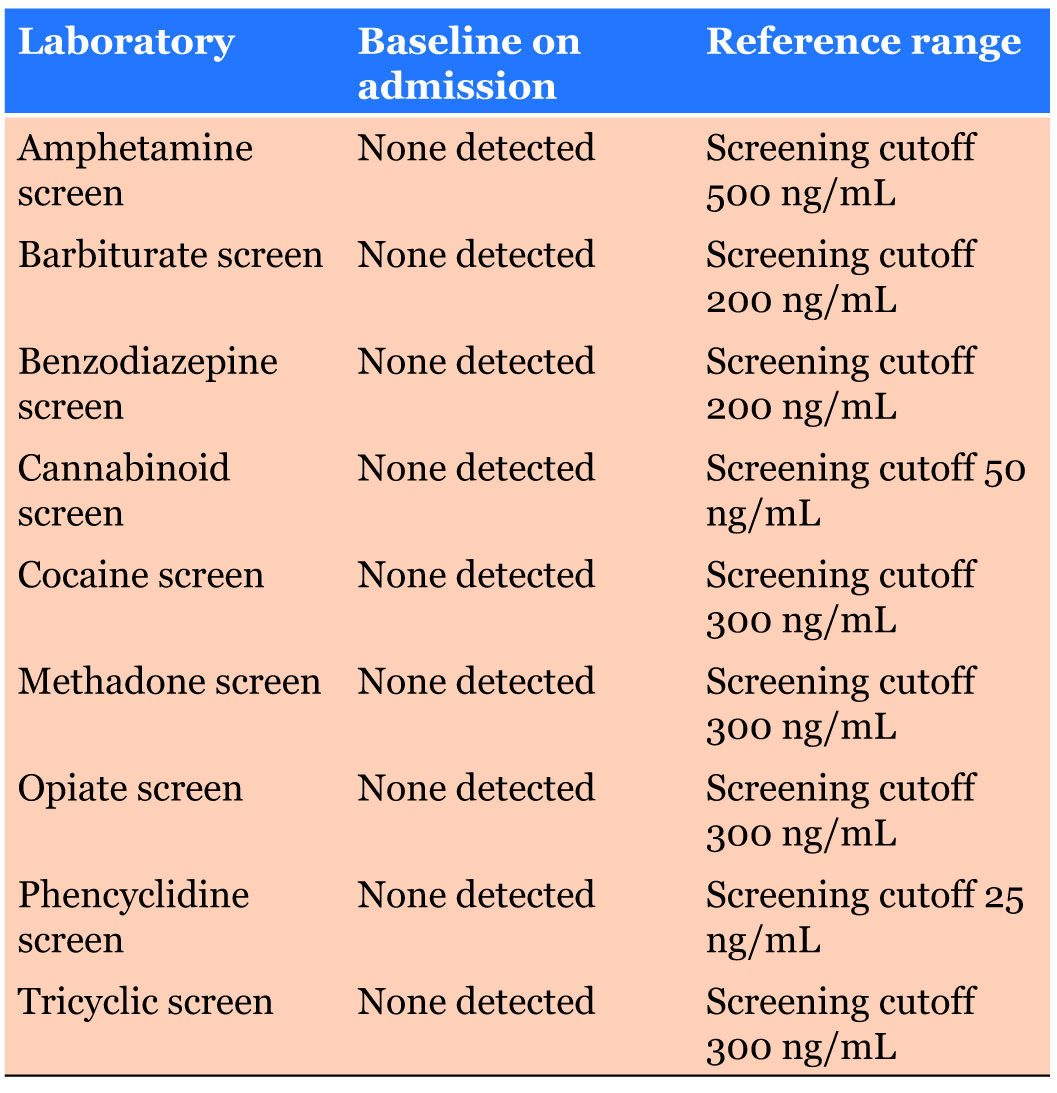
Prior to the ADHD diagnosis, the patient had no known psychiatric or substance abuse history. The urine toxicology screen taken upon admission to the emergency department was positive only for amphetamines. There was no family history of psychotic or mood disorders, and she didn’t exhibit any depressive, manic, or hypomanic symptoms.
The stimulant medications were discontinued by the hospital upon admission to the emergency department and the patient was treated with an atypical antipsychotic. She tolerated the medications well, started psychotherapy sessions, and was released five days later. On the day of discharge, there were no delusions or hallucinations reported. She was referred to the local mental health center for aftercare follow-up with a psychiatrist. [2]
Another powerful case study example is that of Elyn R. Saks, the associate dean and Orrin B. Evans professor of law, psychology, and psychiatry and the behavioral sciences at the University of Southern California Gould Law School.
Saks began experiencing symptoms of mental illness at eight years old, but she had her first full-blown episode when studying as a Marshall scholar at Oxford University. Another breakdown happened while Saks was a student at Yale Law School, after which she “ended up forcibly restrained and forced to take anti-psychotic medication.” Her scholarly efforts thus include taking a careful look at the destructive impact force and coercion can have on the lives of people with psychiatric illnesses, whether during treatment or perhaps in interactions with police; the Saks Institute, for example, co-hosted a conference examining the urgent problem of how to address excessive use of force in encounters between law enforcement and individuals with mental health challenges.
Saks lives with schizophrenia and has written and spoken about her experiences. She says, “There’s a tremendous need to implode the myths of mental illness, to put a face on it, to show people that a diagnosis does not have to lead to a painful and oblique life.”
In recent years, researchers have begun talking about mental health care in the same way addiction specialists speak of recovery—the lifelong journey of self-treatment and discipline that guides substance abuse programs. The idea remains controversial: managing a severe mental illness is more complicated than simply avoiding certain behaviors. Approaches include “medication (usually), therapy (often), a measure of good luck (always)—and, most of all, the inner strength to manage one’s demons, if not banish them. That strength can come from any number of places…love, forgiveness, faith in God, a lifelong friendship.” Saks says, “We who struggle with these disorders can lead full, happy, productive lives, if we have the right resources.”
You can view the transcript for “A tale of mental illness | Elyn Saks” here (opens in new window) .
Candela Citations
- Modification, adaptation, and original content. Authored by : Wallis Back for Lumen Learning. Provided by : Lumen Learning. License : CC BY: Attribution
- A tale of mental illness . Authored by : Elyn Saks. Provided by : TED. Located at : https://www.youtube.com/watch?v=f6CILJA110Y . License : Other . License Terms : Standard YouTube License
- A Case Study of Acute Stimulant-induced Psychosis. Authored by : Ashley Henning, Muhannad Kurtom, Eduardo D. Espiridion. Provided by : Cureus. Located at : https://www.cureus.com/articles/17024-a-case-study-of-acute-stimulant-induced-psychosis#article-disclosures-acknowledgements . License : CC BY: Attribution
- Elyn Saks. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Elyn_Saks . License : CC BY-SA: Attribution-ShareAlike
- A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. Authored by : Yuanhan Bai, Xi Yang, Zhiqiang Zeng, and Haichen Yangcorresponding. Located at : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851085/ . License : CC BY: Attribution
- Bai, Y., Yang, X., Zeng, Z., & Yang, H. (2018). A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. BMC psychiatry , 18(1), 67. https://doi.org/10.1186/s12888-018-1655-5 ↵
- Henning A, Kurtom M, Espiridion E D (February 23, 2019) A Case Study of Acute Stimulant-induced Psychosis. Cureus 11(2): e4126. doi:10.7759/cureus.4126 ↵

This site is intended for healthcare professionals
Schizophrenia case studies: putting theory into practice
This article considers how patients with schizophrenia should be managed when their condition or treatment changes.

DR P. MARAZZI/SCIENCE PHOTO LIBRARY
Treatments for schizophrenia are typically recommended by a mental health specialist; however, it is important that pharmacists recognise their role in the management and monitoring of this condition. In ‘ Schizophrenia: recognition and management ’, advice was provided that would help with identifying symptoms of the condition, and determining and monitoring treatment. In this article, hospital and community pharmacy-based case studies provide further context for the management of patients with schizophrenia who have concurrent conditions or factors that could impact their treatment.
Case study 1: A man who suddenly stops smoking
A man aged 35 years* has been admitted to a ward following a serious injury. He has been taking olanzapine 20mg at night for the past three years to treat his schizophrenia, without any problems, and does not take any other medicines. He smokes 25–30 cigarettes per day, but, because of his injury, he is unable to go outside and has opted to be started on nicotine replacement therapy (NRT) in the form of a patch.
When speaking to him about his medicines, he appears very drowsy and is barely able to speak. After checking his notes, it is found that the nurses are withholding his morphine because he appears over-sedated. The doctor asks the pharmacist if any of the patient’s prescribed therapies could be causing these symptoms.
What could be the cause?
Smoking is known to increase the metabolism of several antipsychotics, including olanzapine, haloperidol and clozapine. This increase is linked to a chemical found in cigarettes, but not nicotine itself. Tobacco smoke contains aromatic hydrocarbons that are inducers of CYP1A2, which are involved in the metabolism of several medicines [1] , [2] , [3] . Therefore, smoking cessation and starting NRT leads to a reduction in clearance of the patient’s olanzapine, leading to increased plasma levels of the antipsychotic olanzapine and potentially more adverse effects — sedation in this case.
Patients who want to stop, or who inadvertently stop, smoking while taking antipsychotics should be monitored for signs of increased adverse effects (e.g. extrapyramidal side effects, weight gain or confusion). Patients who take clozapine and who wish to stop smoking should be referred to their mental health team for review as clozapine levels can increase significantly when smoking is stopped [3] , [4] .
For this patient, olanzapine is reduced to 15mg at night; consequently, he seems much brighter and more responsive. After a period on the ward, he has successfully been treated for his injury and is ready to go home. The doctor has asked for him to be supplied with olanzapine 15mg for discharge along with his NRT.
What should be considered prior to discharge?
It is important to discuss with the patient why his dose was changed during his stay in hospital and to ask whether he intends to start smoking again or to continue with his NRT. Explain to him that if he wants to begin, or is at risk of, smoking again, his olanzapine levels may be impacted and he may be at risk of becoming unwell. It is necessary to warn him of the risk to his current therapy and to speak to his pharmacist or mental health team if he does decide to start smoking again. In addition, this should be used as an opportunity to reinforce the general risks of smoking to the patient and to encourage him to remain smoke-free.
It is also important to speak to the patient’s community team (e.g. doctors, nurses), who specialise in caring for patients with mental health disorders, about why the olanzapine dose was reduced during his stay, so that they can then monitor him in case he does begin smoking again.
Case 2: A woman with constipation
A woman aged 40 years* presents at the pharmacy. The pharmacist recognises her as she often comes in to collect medicine for her family. They are aware that she has a history of schizophrenia and that she was started on clozapine three months ago. She receives this from her mental health team on a weekly basis.
She has visited the pharmacy to discuss constipation that she is experiencing. She has noticed that since she was started on clozapine, her bowel movements have become less frequent. She is concerned as she is currently only able to go to the toilet about once per week. She explains that she feels uncomfortable and sick, and although she has been trying to change her diet to include more fibre, it does not seem to be helping. The patient asks for advice on a suitable laxative.
What needs to be considered?
Constipation is a very common side effect of clozapine . However, it has the potential to become serious and, in rare cases, even fatal [5] , [6] , [7] , [8] . While minor constipation can be managed using over-the-counter medicines (e.g. stimulant laxatives, such as senna, are normally recommended first-line with stool softeners, such as docusate, or osmotic laxatives, such as lactulose, as an alternative choice), severe constipation should be checked by a doctor to ensure there is no serious bowel obstruction as this can lead to paralytic ileus, which can be fatal [9] . Symptoms indicative of severe constipation include: no improvement or bowel movement following laxative use, fever, stomach pain, vomiting, loss of appetite and/or diarrhoea, which can be a sign of faecal impaction overflow.
As the patient has been experiencing this for some time and is only opening her bowels once per week, as well as having other symptoms (i.e. feeling uncomfortable and sick), she should be advised to see her GP as soon as possible.
The patient returns to the pharmacy again a few weeks later to collect a prescription for a member of their family and thanks the pharmacist for their advice. The patient was prescribed a laxative that has led to resolution of symptoms and she explains that she is feeling much better. Although she has a repeat prescription for lactulose 15ml twice per day, she says she is not sure whether she needs to continue to take it as she feels better.
What advice should be provided?
As she has already had an episode of constipation, despite dietary changes, it would be best for the patient to continue with the lactulose at the same dose (i.e. 15ml twice daily), to prevent the problem occurring again. Explain to the patient that as constipation is a common side effect of clozapine, it is reasonable for her to take laxatives before she gets constipation to prevent complications.
Pharmacists should encourage any patient who has previously had constipation to continue taking prescribed laxatives and explain why this is important. Pharmacists should also continue to ask patients about their bowel habits to help pick up any constipation that may be returning. Where pharmacists identify patients who have had problems with constipation prior to starting clozapine, they can recommend the use of a prophylactic laxative such as lactulose.
Case 3: A mother is concerned for her son who is talking to someone who is not there
A woman has been visiting the pharmacy for the past 3 months to collect a prescription for her son, aged 17 years*. In the past, the patient has collected his own medicine. Today the patient has presented with his mother; he looks dishevelled, preoccupied and does not speak to anyone in the pharmacy.
His mother beckons you to the side and expresses her concern for her son, explaining that she often hears him talking to someone who is not there. She adds that he is spending a lot of time in his room by himself and has accused her of tampering with his things. She is not sure what she should do and asks for advice.
What action can the pharmacist take?
It is important to reassure the mother that there is help available to review her son and identify if there are any problems that he is experiencing, but explain it is difficult to say at this point what he may be experiencing. Schizophrenia is a psychotic illness which has several symptoms that are classified as positive (e.g. hallucinations and delusions), negative (e.g. social withdrawal, self-neglect) and cognitive (e.g. poor memory and attention).
Many patients who go on to be diagnosed with schizophrenia will experience a prodromal period before schizophrenia is diagnosed. This may be a period where negative symptoms dominate and patients may become isolated and withdrawn. These symptoms can be confused with depression, particularly in younger people, though depression and anxiety disorders themselves may be prominent and treatment for these may also be needed. In this case, the patient’s mother is describing potential psychotic symptoms and it would be best for her son to be assessed. She should be encouraged to take her son to the GP for an assessment; however, if she is unable to do so, she can talk to the GP herself. It is usually the role of the doctor to refer patients for an assessment and to ensure that any other medical problems are assessed.
Three months later, the patient comes into the pharmacy and seems to be much more like his usual self, having been started on an antipsychotic. He collects his prescription for risperidone and mentions that he is very worried about his weight, which has increased since he started taking the newly prescribed tablets. Although he does not keep track of his weight, he has noticed a physical change and that some of his clothes no longer fit him.
What advice can the pharmacist provide?
Weight gain is common with many antipsychotics [10] . Risperidone is usually associated with a moderate chance of weight gain, which can occur early on in treatment [6] , [11] , [12] . As such, the National Institute for Health and Care Excellence recommends weekly monitoring of weight initially [13] . As well as weight gain, risperidone can be associated with an increased risk of diabetes and dyslipidaemia, which must also be monitored [6] , [11] , [12] . For example, the lipid profile and glucose should be assessed at 12 weeks, 6 months and then annually [12] .
The pharmacist should encourage the patient to attend any appointments for monitoring, which may be provided by his GP or mental health team, and to speak to his mental health team about his weight gain. If he agrees, the pharmacist could inform the patient’s mental health team of his weight gain and concerns on his behalf. It is important to tackle weight gain early on in treatment, as weight loss can be difficult to achieve, even if the medicine is changed.
The pharmacist should provide the patient with advice on healthy eating (e.g. eating a balanced diet with at least five fruit and vegetables per day) and exercising regularly (e.g. doing at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous-intensity activity per week), and direct him to locally available services. The pharmacist can record the adverse effect on the patient’s medical record, which will help flag this in the future and thus help other pharmacists to intervene should he be prescribed risperidone again.
*All case studies are fictional.
Useful resources
- Mind — Schizophrenia
- Rethink Mental Illness — Schizophrenia
- Mental Health Foundation — Schizophrenia
- Royal College of Psychiatrists — Schizophrenia
- NICE guidance [CG178] — Psychosis and schizophrenia in adults: prevention and management
- NICE guidance [CG155] — Psychosis and schizophrenia in children and young people: recognition and management
- British Association for Psychopharmacology — Evidence-based guidelines for the pharmacological treatment of schizophrenia: updated recommendations from the British Association for Psychopharmacology
About the author
Nicola Greenhalgh is lead pharmacist, Mental Health Services, North East London NHS Foundation Trust
[1] Chiu CC, Lu ML, Huang MC & Chen KP. Heavy smoking, reduced olanzapine levels, and treatment effects: a case report. Ther Drug Monit 2004;26(5):579–581. doi: 10.1097/00007691-200410000-00018
[2] de Leon J. Psychopharmacology: atypical antipsychotic dosing: the effect of smoking and caffeine. Psychiatr Serv 2004;55(5):491–493. doi: 10.1176/appi.ps.55.5.491
[3] Mayerova M, Ustohal L, Jarkovsky J et al . Influence of dose, gender, and cigarette smoking on clozapine plasma concentrations. Neuropsychiatr Dis Treat 2018;14:1535–1543. doi: 10.2147/NDT.S163839
[4] Ashir M & Petterson L. Smoking bans and clozapine levels. Adv Psychiatr Treat 2008;14(5):398–399. doi: 10.1192/apt.14.5.398b
[5] Young CR, Bowers MB & Mazure CM. Management of the adverse effects of clozapine. Schizophr Bull 1998;24(3):381–390. doi: 10.1093/oxfordjournals.schbul.a033333
[6] Taylor D, Barnes TRE & Young AH. The Maudsley Prescribing Guidelines in Psychiatry . 13th edn. London: Wiley Blackwell; 2018
[7] Oke V, Schmidt F, Bhattarai B et al . Unrecognized clozapine-related constipation leading to fatal intra-abdominal sepsis — a case report. Int Med Case Rep J 2015;8:189–192. doi: 10.2147/IMCRJ.S86716
[8] Hibbard KR, Propst A, Frank DE & Wyse J. Fatalities associated with clozapine-related constipation and bowel obstruction: a literature review and two case reports. Psychosomatics 2009;50(4):416–419. doi: 10.1176/appi.psy.50.4.416
[9] Medicines and Healthcare products Regulatory Agency. Clozapine: reminder of potentially fatal risk of intestinal obstruction, faecal impaction, and paralytic ileus. 2020. Available from: https://www.gov.uk/drug-safety-update/clozapine-reminder-of-potentially-fatal-risk-of-intestinal-obstruction-faecal-impaction-and-paralytic-ileus (accessed April 2020)
[10] Leucht S, Cipriani A, Spineli L et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 2013;382(9896):951–962. doi: 10.1016/S0140-6736(13)60733-3
[11] Bazire S. Psychotropic Drug Directory . Norwich: Lloyd-Reinhold Communications LLP; 2018
[12] Cooper SJ & Reynolds GP. BAP guidelines on the management of weight gain, metabolic disturbances and cardiovascular risk associated with psychosis and antipsychotic drug treatment. J Psychopharmacol 2016;30(8):717–748. doi: 10.1177/0269881116645254
[13] National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: prevention and management. Clinical guideline [CG178]. 2014. Available from: https://www.nice.org.uk/guidance/cg178 (accessed April 2020)

You might also be interested in…

Schizophrenia: symptoms, diagnosis and treatment

Nearly half of long-term antidepressant users could safely taper off medication using helpline

Boots UK shuts online mental health service to new patients

Edorium Journals
- About Edorium Journals
- Browse Journals
- Abstracting & Indexing
- Testimonials
Article Outline
- Introduction
Case Report
- Supporting Information
Related Articles
“one in a million”: a case of a very early onset schizophrenia.
1 Assistant Professor of Psychiatry, Department of Psychiatry, Penn State Health Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA
2 PGY4-Child and Adolescent Psychiatry Fellow, Department of Psychiatry, Penn State Health Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA
Address correspondence to:
Daisy Vyas Shirk
DO, 875 Stoverdale Road, Hummelstown, Pennsylvania 17036,
Message to Corresponding Author
Article ID: 100083Z06DS2020
doi: 10.5348/100083Z06DS2020CR
Access full text article on other devices
Access pdf of article on other devices, how to cite this article.
Introduction: Very early onset schizophrenia (VEOS), psychosis prior to age 13, is rare with an incidence of less than 0.04%. Its clinical presentation, course, and outcome differ from early onset (ages 13–18) and adult onset (ages 18 and up) schizophrenia. It is associated with poor response to treatment, poorer prognosis, and multiple hospitalizations. Early identification and intervention has shown to improve overall functioning.
Case Report: We present a case of a 12-year-old female with significant family history of psychosis, admitted due to physical and verbal aggression, sexual inappropriateness, destruction of property, response to internal stimuli, decline in functioning, and 10 month history of social isolation. She responded to risperidone treatment. The patient was discharged to partial hospitalization program but could not tolerate the group setting resulting in discharge to outpatient services. Psychosocial supports were put in place to help with environmental and family dynamics to improve outcome.
Conclusion: As per a recent study, one-third of children and adolescents with psychosis initially present with negative symptoms. It has also been reported that 30% of those with negative symptoms develop treatment failure with antipsychotics. Given these statistics and the treatment challenges of this case, it was imperative to provide additional psychosocial supports to the patients and families, to improve overall functioning and long-term prognosis.
Keywords: Compliance, Intellectual disability, Psychotic disorders, Psychosocial support systems
INTRODUCTION
Very early onset schizophrenia (VEOS), defined as onset of psychosis prior to age 13, is considered to be very rare [1] . It has been shown to differ in its clinical presentation, course, and outcome compared to early onset (between ages 13 and 18) and adult onset (ages 18 and up) schizophrenia. It is associated with poorer prognosis, worse overall functioning, and multiple hospitalizations [2] . Early childhood adversity and borderline intellectual functioning have also been shown to contribute to development of psychosis [3] , [4] , [5] . Early identification and intervention have been shown to reduce the morbidity of the illness and improve overall functioning. Here we present the case of a young girl with very early onset schizophrenia.
CASE REPORT
This is a case of a 12-year-old female child who was admitted in the inpatient child psychiatry unit due to physical and verbal aggression toward peers and staff, sexually inappropriate touching, destruction of property, attempting to run out into traffic, and responding to internal stimuli.
The patient was reportedly doing well until 10 months prior to her hospitalization, after which she exhibited school refusal and declining grades. The only trigger reported was school bullying. She was noted to become more verbally and physically aggressive toward peers and school staff, with daily outbursts, eloping from school, poor sleep, and social isolation. At home, she was observed to sit in the halls in the middle of the night, conversing with herself. She changed from a child who “used to love talking, playing board games, and card game with her cousins” into someone who “now sits by herself and does not say anything to them or do anything with them.” She was also found one time sitting on her porch eating leaves.
She was referred and underwent partial hospitalization. During that treatment, she was observed to be impulsive, hyperactive, withdrawn, had difficulty with peer interactions, appeared internally preoccupied, laughed inappropriately, talked to herself, sing, or would dance alone without music. She struggled with boundaries and attempted few times to choke staffs with their lanyards or with her hands. She destroyed property, made verbal threats toward staff and peers, and made sexually inappropriate comments and gestures. She was given a trial of lithium and risperidone. She did not tolerate lithium but responded to risperidone 1 mg daily. Upon discharge, there was no follow-up and patient ran out of medication. This led to a deterioration of behaviors resulting in inpatient treatment.
Patient’s developmental history and medical histories are unremarkable. Her family history is significant for schizophrenia in her father who reportedly went from being a straight A student, attending college on a full scholarship to dropping out of school, having multiple incarcerations and now has been institutionalized in a long-term psychiatric facility for the past 10 years. The patient’s mother also received inpatient treatment after patient’s birth and there was a threat of all three children being removed by Children and Youth Services (CYS). At the time of hospitalization, she lived with her mother, 9-year-old sister, and 3-year-old brother. Child protection services were involved at the time of admission due to concerns of a possible sexual abuse based on patient’s sexualized behaviors.
Mental status examination at the time of admission
The patient had fair grooming but was agitated and uncooperative during the interview. Her eye contact varied from fair to intense staring. She did not display any motor abnormalities including tics or tremors. She spoke loudly and often repeated the phrase, “I don’t give a f***” to many questions. She refused to describe her mood and her affect was bizarre and labile; though content was characteristic of paranoia and perseverations. She refused to answer questions related to perceptual disturbances, suicidality, and homicidality. Her orientation, memory, and knowledge could not be fully assessed. Her attention, insight, and judgment were impaired.
Admission diagnosis
Unspecified psychosis was not revealed due to a substance or known physiological condition.
Course of inpatient treatment
The patient was diagnosed with unspecified psychosis on admission. Workup ( Table 1 , Table 2 , Table 3 , Table 4 , Table 5 , Table 6 ) was done and the patient was restarted on risperidone for her aggression and hallucinations. On her first three days of hospitalization, she displayed aggressive, impulsive, and disruptive behaviors toward peers and staffs. Her risperidone was titrated up to 1.75 mg/day. Her aggression subsided and she was able to attend groups. However, she had difficulty engaging with others, often preferring to sit by herself and away from the crowd. She initially endorsed auditory and visual hallucinations where she saw shadows or gravesite with numbers. She would occasionally have difficulty distinguishing reality from fiction, often asking staff if they were real or part of her imagination. Early on in her treatment, the patient had several days when she reported “itching” on her chest stating that she was being stabbed by someone. Once that was resolved, she became preoccupied by her fingertips and would often be seen picking at the tips of her fingers. She struggled with being able to process information and was often mute or would repeat things that had been said to her or perseverate on a specific sentence. She displayed paranoia on the unit, often worrying that someone would come in and hurt her and at times feared that the staff would hurt her. Initially, she had trouble sleeping at night and would often stand in her doorway staring at staff for the majority of the night. She was allowed to sleep on a mattress in her doorway which seemed to help at times but not consistently. Later, she denied having hallucinations although she appeared internally preoccupied throughout the stay.
Neuropsychological assessment was completed which revealed that the patient’s IQ was likely in the borderline range (70–79). She had limited verbal comprehension and expression, relative weakness in verbal knowledge, fluid reasoning, set-shifting, visual-motor integration, phonemic and semantic fluency, and rote verbal memory. She also had significant deficits in executive functioning and negative and positive symptoms of psychosis.
Medical issues
Started on Vitamin D3 to correct for low Vitamin D.
Interventions at discharge
Due to the many challenges this patient presented and concerns about compliance with aftercare recommendations, she was referred to as many outpatient services as possible to help improve her prognosis. These services included partial hospitalization, involvement of children and youth services, case management services, family support in the form of patient’s paternal grandmother, referral for electroencephalogram (EEG) and magnetic resonance imaging (MRI) of brain and school involvement.
Partial hospital treatment
Upon arrival to partial hospitalization, patient’s behaviors had deteriorated due to non-compliance with medications for a week as a result of problem with insurance. She reported sporadic hallucinations, giggled by herself, displayed thought blocking, disorganized behaviors, made random, unrelated, bizarre statements, sometimes loudly and perseverated on them and was paranoid.
During her partial hospitalization, she was disruptive, made sexually inappropriate comments and became verbally and physically aggressive toward staff. As a result of these behaviors and her inability to tolerate the group setting of partial hospitalization, she had to be discharged to outpatient services. As was the case during her discharge from inpatient treatment, patient’s mother did not show up for her discharge and CYS had to find her.
When found, her mother once again claimed she was unaware of the discharge.
Follow-up in outpatient treatment
In the outpatient clinic, risperidone was titrated up to 1 mg orally twice a day, with a good response. Patient’s mother reported that the patient was doing well in school and seemed to be at her baseline after dose increase. During outpatient visits, the patient denied hallucinations, thought blocking was noted to improve, and the patient was answering questions and smiling appropriately most of the times.
Response latency and processing time remained slow but showed improved from previous visits. Family based mental health (FBMHS) services were recommended and started with in-home therapy 2–3 times a week. A case manager through CYS was recommended to support family in managing follow-up appointments.
Share Image:
Very early onset psychosis, defined as psychosis before the age of 13, is an extremely rare occurrence with an incidence of less than 0.04% [1] , [6] . One-third of children and adolescents with psychosis initially present with negative symptoms and 30% of those who present with negative symptoms at baseline go on to develop treatment failure with antipsychotics. Confounding these statistics is that VEOS is often difficult to diagnose, especially in this case due to lack of reliable collateral information from family. Our patient presented with several risk factors including father’s diagnosis of schizophrenia requiring institutionalization for the past 10 years. There was also a strong suspicion of mental illness in patient’s mother. Environmentally, our patient had a history of trauma in the form of bullying at school and she lacked social supports and lack of follow-up with treatment recommendations.
Additionally, our patient had several premorbid symptoms such as social withdrawal, poverty of speech, and steady decline in social and academic performance over the course of her educational history. Freeman et al. [4] have reported that there is a direct correlation between lower intellectual functioning and development of psychosis due to alteration in the way stimuli and events are interpreted. Another study demonstrated a significant association with psychosis and auditory hallucinations “that remained significant after controlling for age, gender, current social class and ethnicity” [5] . Childhood adversity, as experienced by this patient, also increases the risk of psychosis. A review by Varese et al. [3] showed that exposure to all types of adversity (except parental death) was related to an increased risk of psychosis. Furthermore, a recent study of adolescents experiencing psychosis suggested early intervention by a specialist team may improve treatment outcomes in both positive and negative symptoms [7] . This may also hold true for VEOS. At presentation, our patient displayed the following negative symptoms of schizophrenia: blunted affect, emotional withdrawal, poor rapport, social isolation, poverty of speech, mutism, and psychomotor retardation.
Comorbidities for this patient included oppositional defiant behaviors, borderline intellectual functioning and trauma in the form of physical and emotional abuse by peers, and suspicion of possible sexual abuse given her sexual acting out behaviors.
Our patient provided several treatment challenges due to her mother’s mental state and inability to provide reliable collateral information, non-compliance with follow-up with patient’s outpatient services, and non-compliance with following medication recommendations. Additionally, the lack of sufficient services for young children with psychosis made aftercare recommendations challenging for the treatment team.
Given the many complications this patient presented, the treatment team focused on utilizing the resources that were available such as patient’s paternal grandmother’s increased involvement in her care. There was also collaboration of care with outside agencies such as Children and Youth Services, Case Management, and her school. These services provided support to her mother and made her accountable for complying with aftercare plans and recommendations.
One-third of children and adolescents with psychosis initially present with negative symptoms and 30% of those with negative symptoms, develop treatment failure with antipsychotics. Given these statistics and the treatment challenges of treating children with psychosis, it is imperative to provide additional psychosocial supports to the patients and families, to improve overall functioning and long-term prognosis. This case presents an excellent example of many challenges that are faced in treating early onset psychosis.
SUPPORTING INFORMATION
Daisy Vyas Shirk - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Meenal Pathak - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jasmin Gange Lagman - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Khurram S Janjua - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The corresponding author is the guarantor of submission.
Written informed consent was obtained from the patient for publication of this article.
All relevant data are within the paper and its Supporting Information files.
Authors declare no conflict of interest.
© 2020 Daisy Vyas Shirk et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.
Comment on Article
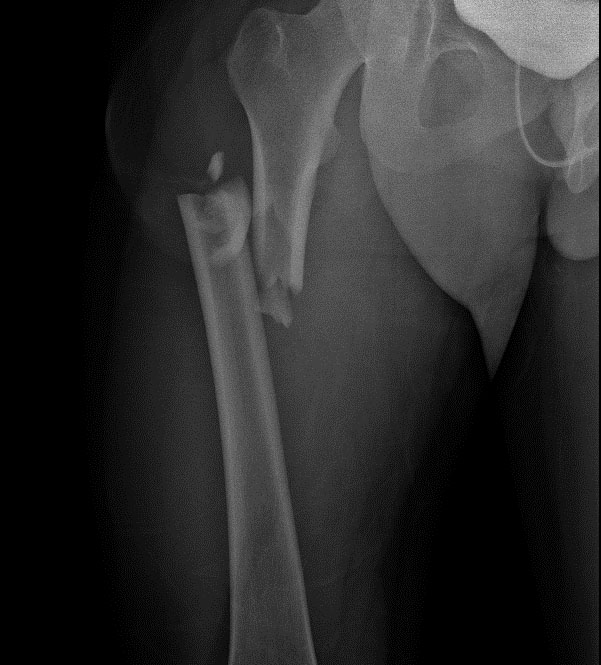
Pulmonary embolism identified prior to anesthesia induction in a low-risk patient
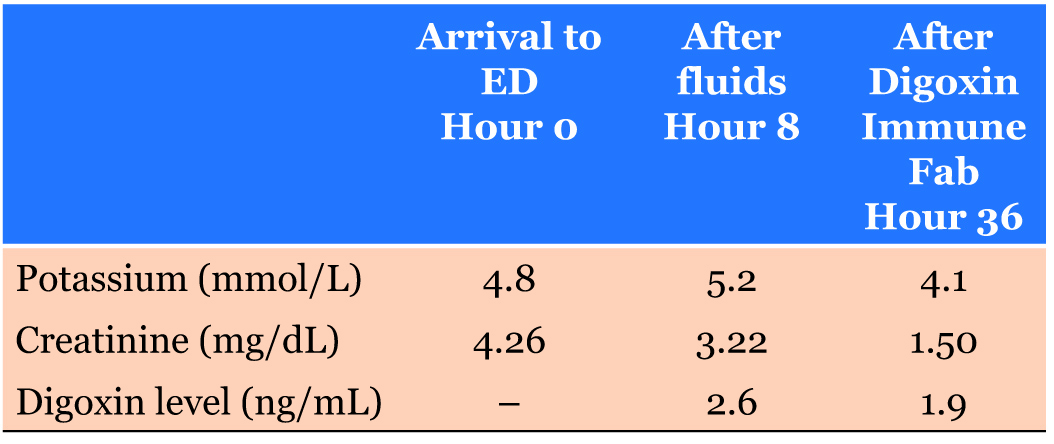
Fatal arrhythmias despite early recognized successful treatment of digoxin toxicity

Unusual presentation of giant schwannoma in the sciatic nerve
- Article Access
- Abstract HTML
- Full Text PDF
- Full Text XML
- Download PDF
- Download Citation
- Print Article
- Share Article
- Via Facebook
- Via Twitter
- Via LinkedIn
Page Views: 2429
PDF Downloads: 111
XML Downloads:
ePub Downloads:
Citations: 0
Reader Comments: 0
- Subject Areas
Message To Corresponding Author

IMAGES
VIDEO
COMMENTS
Another powerful case study example is that of Elyn R. Saks, the associate dean and Orrin B. Evans professor of law, psychology, and psychiatry and the behavioral sciences at the University of Southern California Gould Law School. ... Saks lives with schizophrenia and has written and spoken about her experiences. She says, "There's a ...
In the current case study of the 26 year old male student diagnosed with paranoid schizophrenia we discuss the possible consequences of a short break in the therapeutic process on the treatment ...
We report a case involving a young African male adult with gainful employment and no history of substance abuse who was diagnosed with schizophrenia. The patient was referred to the psychiatric unit of a hospital, and interventions by clinical pharmacists during management of the patient's medical problems contributed to overall improved ...
Case study 1: A man who suddenly stops smoking. A man aged 35 years* has been admitted to a ward following a serious injury. He has been taking olanzapine 20mg at night for the past three years to treat his schizophrenia, without any problems, and does not take any other medicines.
as I felt that presenting a real clinical case was the best way to depict the dimension of complexity in understanding and assist-ing the person affected by this psychiatric pathology. The case examined concerns the story of L., a 28-year-old boy, suffering from schizophrenia for 10 years, hospitalized numerous times in SPDC.
Introduction: Very early onset schizophrenia (VEOS), psychosis prior to age 13, is rare with an incidence of less than 0.04%. Its clinical presentation, course, and outcome differ from early onset (ages 13-18) and adult onset (ages 18 and up) schizophrenia. It is associated with poor response to treatment, poorer prognosis, and multiple hospitalizations.
A case study in adolescent's schizophrenia Matt, a 15 years, 6 month old boy, was referred simultaneously by his General Practitioner and the crisis intervention team. He had been found in a park wandering and had been reported to the police by onlookers. When the police arrived on the scene and questioned him, he had
Mona Zein, "Case Study of Schizophrenia in A Young Adult Male." American Journal of Applied Psychology, vol. 10, no. 1 (2022): 20-30. doi: 10.12691/ajap-10-1-4. 1. Introduction . Schizophrenia is a severe and chronic mental illness that affects approximately 1% of the population, characterized by a complex of clinical syndromes and a
This single case study describes a structural therapy perspective applied to a family and examines interaction patterns within the clinical setting and the home; the therapeutic view examines contextual variables that affect an individual diagnosed with schizophrenia, his family, and his recovery.
severe and persistent problems that characterize schizophrenia. This case study describes the process of CBT in the long-term outpatient care of a young woman with schizophrenia. The study highlights the adaptation of cognitive-behavioural strategies to the unique needs of schizophrenia and presents data regarding clinical outcomes in this case.